Liver Cancer
Liver cancer is cancer that starts in your liver. There are different kinds of liver cancer. But the most common type in adults is called hepatocellular carcinoma. It starts in the main liver cells called hepatocytes.
Why choose us?
Saint Luke’s Cancer Specialists provide early detection, expert diagnosis, personalized treatment options, and survivorship support to every patient.
We offer comprehensive treatment options. If surgery or transplant is needed, the Saint Luke’s Liver Biliary & Pancreatic Center provides expert surgical care for liver cancer patients. Highly specialized interventional radiologists and radiation oncologists provide non-surgical treatment options.
Saint Luke’s provides comprehensive, state-of-the-art services for the treatment of liver cancer. Our team provides the latest diagnostic and to patients with all stages of liver cancer.
Liver cancer is a complex disease. It occurs as a complication of liver disease and cirrhosis. Liver cancers are also more prevalent in men infected with hepatitis B or C, and the risk factors increase for individuals who smoke or consume excessive amounts of alcohol.
Saint Luke’s takes a multidisciplinary approach to diagnosing and treating this disease.
Treatment options
- Chemoembolization
- Alcohol ablation
- Radiofrequency ablation
- Cryotherapy
- Laparoscopic resection/ablation
TransArterial RadioEmbolization (TARE)
If you have cirrhosis, there are actions you can control which may reduce your chances of developing liver cancer:
- Stop smoking
- Stop drinking alcohol, including nonalcoholic beer
- Consider undergoing treatment if you have viral hepatitis
Liver Cancer Introduction
What is cancer?
Cancer starts when cells in the body change (mutate) and grow out of control. Your body is made up of tiny building blocks called cells. Normal cells grow when your body needs them and die when your body doesn't need them any longer.
Cancer is made up of abnormal cells that grow even though your body doesn't need them. In most cancers, the abnormal cells grow to form a lump or mass called a tumor. If cancer cells are in the body long enough, they can grow into (invade) nearby areas. They can even spread to other parts of the body (metastasize).
What is liver cancer?
Liver cancer is cancer that starts in your liver. It's also called primary liver cancer. Primary liver cancer is not the same as cancer that started somewhere else in the body and then spread (metastasized) to the liver. Cancer that starts in another organ, such as the colon, breast, or lung, and then spreads to the liver is called secondary liver cancer. Secondary liver cancer is far more common in the U.S. than primary liver cancer. Cancer that has spread to the liver from somewhere else is treated like the original cancer. For instance, lung cancer that has spread to the liver is treated like lung cancer.
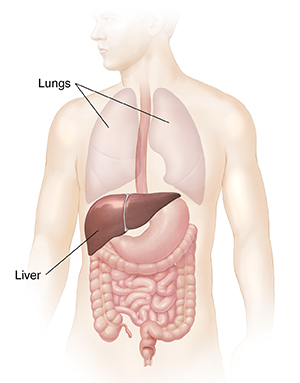
Understanding the liver
The liver is a large, pyramid-shaped organ that lies behind your ribs on the right side of your body. It’s under the right lung. It's divided into right and left lobes.
The liver helps break down and store nutrients. These include sugars, starch, fats, and proteins. It also makes proteins, such as albumin. This helps the body balance fluids. The liver makes clotting factors, which help blood get thick or clot when a person is bleeding. Bile made in the liver is important for digesting food and for other bodily functions.
One of the liver’s most important jobs is to filter out and destroy toxins in the blood. When the liver isn’t working well, chemicals can build up inside the body and cause damage.
What types of cancer start in the liver?
The main types of primary liver cancer include:
- Hepatocellular carcinoma. This is the most common liver cancer. About 4 out of every 5 primary liver cancers are this type. It starts in the main liver cells called hepatocytes.
- Intrahepatic cholangiocarcinoma (bile duct cancer). About 1 in 10 to 1 in 5 liver cancers are cholangiocarcinomas. These cancers start in the bile ducts. These are small tubes that carry bile out of the liver and into the gallbladder and intestines during digestion. This type of cancer can also start in the bile ducts outside the liver.
- Hepatoblastoma. This is a very rare liver cancer. It's most often found in young children.
- Angiosarcoma. This is another rare form of liver cancer. It starts in blood vessels inside the liver.
Several types of noncancer (benign) tumors can also form in the liver. These include hemangiomas, hepatic adenomas, and focal nodular hyperplasia. These tumors don’t spread to other parts of the body. But they can still cause problems if they grow large enough.
Talk with your healthcare provider
If you have questions about liver cancer, talk with your healthcare provider. Your healthcare provider can help you understand more about this cancer.
What is a risk factor?
A risk factor is anything that may increase your chance of having a disease. Risk factors for a certain type of cancer might include smoking, diet, family history, or many other things. The exact cause of someone’s cancer may not be known. But risk factors can make it more likely for a person to have cancer.
Things you should know about risk factors for cancer:
- Risk factors can increase a person's risk, but they don't always cause the disease.
- Some people with risk factors never get cancer. Other people with cancer have few or no known risk factors.
- Some risk factors are very well known. But there's ongoing research about risk factors for many types of cancer.
Some risk factors, such as family history, may not be in your control. But others may be things you can change. Knowing about risk factors can help you make choices that might lower your risk. For example, if an unhealthy diet is a risk factor, you may choose to eat healthy foods. If excess weight is a risk factor, you may decide to lose weight.
Who is at risk for liver cancer?
Anyone can get liver cancer. But there are some factors that can increase your risk for it. These include:
- Chronic viral hepatitis. Worldwide, chronic hepatitis B virus (HBV) and hepatitis C virus (HCV) infections are the biggest risk factors for liver cancer. These viruses can cause inflammation that can lead to scarring or cirrhosis.
- Alcohol abuse. People who drink a lot of alcohol are at increased risk for cirrhosis. This raises their risk for liver cancer.
- Obesity. People who are very overweight are at higher risk for liver cancer.
- Cirrhosis. People who have scarring of their liver, whether it’s from hepatitis, alcohol use, or some other cause, have a higher risk for liver cancer.
- Type 2 diabetes. People with type 2 diabetes have a higher risk for liver cancer. This might be because they tend to be overweight or obese.
- Exposure to certain chemicals. Chemicals that have been linked to liver cancer include arsenic in drinking water, vinyl chloride, thorium dioxide (Thorotrast), and anabolic steroids. They also include aflatoxins. Aflatoxins are made by a mold that can grow on stored grains and nuts.
- Smoking. People who smoke have a higher risk for liver cancer.
What are your risk factors?
Talk with your healthcare provider about your risk factors for liver cancer. Ask what you can do about them. Some risk factors might not be under your control. But there are some things you can do that might help lower your risk:
- Don't do activities that increase your risk for HBV and HCV infection. Don’t use intravenous drugs, don’t have many sex partners, and don’t handle human blood or fluids without protection. All of these increase your risk of getting these viruses. Also ask your healthcare provider if you should get the hepatitis B vaccine. If you’re at risk for HBV or HCV infection, ask your healthcare provider about getting tested. For people who are infected, medicines can often keep the infections in check or even cure them. This may lower your risk for liver cancer.
- Limit or stay away from alcohol. It's best not to drink alcohol. Men who drink should limit themselves to two drinks or fewer per day. Women who drink should limit themselves to one drink or fewer per day.
- Get to and stay at a healthy weight. Ask your healthcare provider for help if needed.
- Don't smoke. If you smoke, get help to quit.
If you have a high risk for liver cancer because of cirrhosis or other reasons, your healthcare provider may test you regularly for liver cancer. Blood tests and ultrasounds can be used to look for early signs of liver cancer. If you think you might be at high risk, talk with your healthcare provider.
Liver cancer often does not cause symptoms in its early stages, when it's small and hasn't spread. In fact, many liver cancers don't cause symptoms until they have grown fairly large.
People with liver cancer may have these symptoms:
- Unplanned weight loss
- Change in eating habits. This may be a sudden loss of appetite that lasts for a long time or feeling very full even after very small meals.
- Nausea or vomiting
- A lump or mass in the upper-right side of your belly (abdomen). Your liver might become enlarged. This can sometimes be felt as a lump or mass under your right ribs.
- Belly pain. Some people might also have pain at the right shoulder blade.
- Abdominal swelling. This can be caused by fluid building up in your abdomen (called ascites). Some people may have enlarged veins on their belly, too.
- Jaundice or itching. Yellowing of the whites of your eyes and skin (jaundice) is caused by the buildup of too much bilirubin in your blood. This is a chemical made by the liver. Too much of it can also cause severe itching.
- Fever
- Easy bleeding and bruising
- Feeling very tired or weak
When to see your healthcare provider
Many of these symptoms can be caused by other health problems. Still, it's important to see a healthcare provider if you have these symptoms. Only a healthcare provider can tell if you have liver cancer.
Treatment Choices
There are many types of treatment for liver cancer. The one that's best for you depends on things such as:
- The type of cancer
- The size of the tumor
- Extent of the disease, called the stage
- Your age
- Your overall health
- How well the rest of your liver is working
- Your personal concerns and preferences, like what side effects you’ll find acceptable
Learning about your treatment choices
You may have questions and concerns about your treatment choices. You may want to know how you’ll feel during treatment, how your body will work after treatment, and if you’ll have to change your normal activities.
Your healthcare provider is the best person to answer your questions. They can explain what your treatment choices are, how well treatment is expected to work, what the risks and side effects may be, and what the goal of treatment is.
Your healthcare provider may advise a certain treatment. Or they may offer more than one and ask you to decide which one you’d like to use. It can be hard to make this decision. It’s important to take the time you need to make the best decision.
Deciding on the best plan may take some time. Talk with your healthcare provider about how much time you can take to explore your choices. You may want to get a second opinion before deciding on your treatment plan. You may also want to involve your partner, spouse, family, or friends in this process.
Goals of treatment for liver cancer
For some liver cancers, the goal of treatment is to cure the cancer. If a cure isn’t possible, treatment may be used to shrink the cancer or keep it under control. Treatment can also improve your quality of life by helping to control symptoms caused by the cancer. The goal of liver cancer treatment is to do one or more of these things:
- Remove the cancer in the liver (or the entire liver) while doing as little damage as possible to nearby areas
- Kill cancer cells or keep them from growing or spreading
- Keep the cancer from coming back or delay its return
- Ease symptoms of the cancer, such as pain or blockages
Each type of treatment has a different goal. Talk to your healthcare provider about treatment goals so you know what to expect.
Types of treatment for liver cancer
Treatment for cancer is either local or systemic. You may have both.
Local treatments remove, destroy, or control cancer cells in a certain place in the body. Surgery and ablation are local treatments.
Systemic treatments destroy or control cancer cells throughout the body. Immunotherapy, targeted therapy, and chemotherapy are examples.
Commonly used treatments for liver cancer
Here is an overview of the most common treatments for liver cancer.
Surgery
Surgery offers the best chance to cure liver cancer. But only a few people can have surgery. If the cancer is small and in only one part of the liver (and the rest of the liver is healthy enough), the part of the liver with the cancer can be removed. This surgery is called a partial hepatectomy.
Another choice might be to remove the entire liver and replace it with a liver transplant. Again, the cancer must be only in the liver. It can't be in nearby tissues or other parts of the body, and a donated liver must be found.
Tumor ablation and embolization
These methods can be used to treat some tumors in the liver. Ablation involves using heat (radiofrequency ablation or RFA), cold (cryoablation), or other methods to destroy tumors instead of removing them.
Embolization is used to cut off a tumor's blood supply. A substance is injected into the blood vessel going to the tumor. Sometimes this is combined with radiation (radioembolization) or chemotherapy (chemoembolization). In this case, the radioactive particles or chemo are put through the blood vessel into the tumor and then the blood vessel is blocked off. This traps the radiation or chemo in the tumor and cuts off the blood supply. Both of these things kill cancer cells.
Radiation
Radiation uses high-energy X-rays to kill cancer cells. It’s used mainly when surgery can't be done or other treatments aren't good methods. It might be used to treat tumors that have spread and are causing problems in other parts of the body, like the bones or brain.
Targeted therapy
This type of treatment uses medicines that target certain proteins, genes, or cell functions that help cancer cells grow. It’s used mainly for liver cancers that can't be removed with surgery.
Immunotherapy
These medicines help your immune system find and kill cancer cells. Some liver cancer cells use a protein called PD-L1 to keep your immune system from attacking them. Medicines that block PD-L1 can boost the immune system against these cancer cells. CTLA-4 is another protein liver cancer cells use. Medicines can block this protein so the immune system can kill the cells.
Chemotherapy
The goal of chemotherapy (chemo) is to stop cancer from growing or spreading. Strong medicines are used to kill the cells or stop them from dividing. Chemo doesn't work very well for liver cancer, but it may be used to treat advanced liver cancer.
Supportive care
Your healthcare provider may suggest treatments that help ease your symptoms, but don’t treat the cancer. These can sometimes be used along with other treatments. Or your healthcare provider may suggest supportive care if they think that available treatments are more likely to do you more harm than good.
Clinical trials for new treatments
Researchers are always looking for new ways to treat liver cancer. These new methods are tested in clinical trials. Taking part in a clinical trial means you get the best treatment available today, and you might also get new treatments that are thought to be even better. Before starting treatment, talk with your healthcare provider to find out if there are any clinical trials you should think about.
Talking with your healthcare provider
At first, thinking about treatment choices may seem overwhelming. Talk with your healthcare team and loved ones. Make a list of questions. Consider the benefits and side effects of each choice. Discuss your concerns with your healthcare provider before making a decision.