What Is Continuous Glucose Monitoring (CGM)?
Continuous glucose monitoring (CGM) is a way to constantly track your blood sugar. It’s done with a device that has sensors put under your skin. It checks the sugar level in the fluid between your body cells. The sensors send readings to a monitor or your cell phone every few minutes. It does this all day and night. It can help you know if your blood sugar is on the rise or is dropping. This can help you balance food, activity, and insulin. You can have better control over your diabetes. Some monitors have an alarm you can set if your blood sugar reaches a certain level.
Even children can use CGM. Blood sugar readings can be sent to a parent’s or caregiver’s monitor or phone. It can alert parents to a child’s dropping blood sugar during the night so they can help.
Some CGM systems can stop the need for finger sticks. Other CGM systems can reduce how often you need to do a finger stick. Both types still rely on standard blood sugar monitoring to make sure the system is set up correctly.
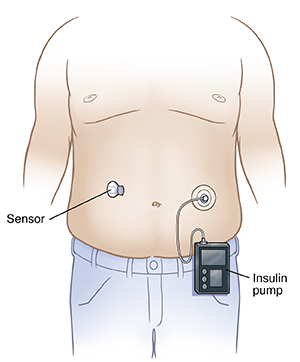
The sensor is usually put on the back of the upper arm. Or it may be put on the belly or back. In some cases, a CGM can sync with an insulin pump. Some insulin pumps can use CGM information to automatically change your insulin dose.
Why might I need CGM?
CGM can help manage type 1 diabetes and type 2 diabetes in some people. Your provider may advise using a CGM device if you are newly diagnosed and need to take insulin. It’s ideal for people who need to have tight blood sugar control. It can help them keep blood sugar from getting too high or too low. And it can help people who may not notice symptoms of low blood sugar.
CGM can help you see trends in your diabetes management. For example, you may notice that your blood sugar is lower at certain times of the day or after certain activities. You can start to make better choices about what to eat and how much activity you can safely do. You can find out if you need to change your insulin dose. Your healthcare provider may set you up with a CGM system for a few days to see your blood sugar patterns before giving any new advice for your care. That way you could try more than 1 CGM system before deciding.
What is time-in-range?
CGM has become more popular and more exact over the years. And there are new ways to manage your blood sugar. Time-in-range is the amount of time you spend in your target blood sugar range. The target is between 70mg/dL and 180 mg/dL for most people.
This measurement looks at the CGM data. It detects how long you have been in range. It will show how long you have been high (hyperglycemia) or low (hypoglycemia). This data can help you know what foods and what activity level causes your blood sugar to rise and fall.
Most people with type 1 and type 2 diabetes aim for a time-in-range of 70%. This means 70% of the time you are in your target range. Staying in this 70% time-in-range can help lower your risk of some complications.
Are there drawbacks to CGM?
CGM does not always replace pricking your finger and testing a drop of blood with a standard glucose meter. You may need a standard monitor to check the CGM readings before making any changes or if you have a hypoglycemic event. If you are getting your CGM results on your smartphone, be sure you can still get alerts about low blood sugars when your phone is on vibrate or on other settings.
CGM costs more than a standard monitor. Some insurance plans don’t cover the cost of a CGM.
CGM gives a lot of data. Some people may find it’s too much information. They may prefer a simpler approach. The various models of CGM machines can be quite different from each other. So be sure the training you get is for your CGM machine.
Wearing a device day and night can be a problem for some people. They may react to the adhesive used to hold the device on the skin.
All CGMs have parts that need to be replaced from time to time. You will need to replace the sensor every 7 to 14 days. Check with your healthcare provider or the maker of your device about when to replace the sensor. This may vary based on which device you use.
You may be asked to remove the sensor before having X-rays or an MRI. If you need to remove the sensor, bring a new one with you to your appointment. Try to schedule your appointment when it's time to replace your sensor.