Understanding Vulvectomy
Vulvectomy is surgery to remove some or all of a woman's outer genitals (called the vulva). This surgery is sometimes needed to treat vulvar cancer or precancer, as well as other diseases of the vulva.
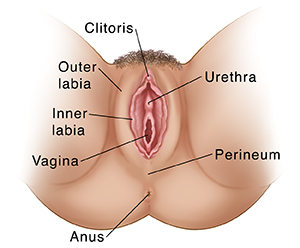
The vulva area has many parts. These include the inner and outer labia (lips) of the vagina, the opening of the vagina, and the clitoris. The vulva also includes the opening of the urinary tract (urethra) and the perineum, which is the skin between the vaginal opening and the anus.
Vulvectomy can be done in many ways. It depends on how big the tumor is, how deep it is, and how much tissue is affected. The goal is to remove all of the cancer along with an edge (margin) of healthy tissue around it. If possible, the clitoris is left in place. Sometimes a skin graft is needed. This means skin is taken from another part of your body and moved to cover the area where skin was removed from your vulva.
There are mainly two ways to describe a vulvectomy procedure:
- Total or partial, to describe the amount of vulvar tissue removed.
- Superficial or skinning, simple, or radical, to describe the depth of the tissue (below the skin) that must be removed.
Some of the common types of vulvectomy include:
- Wide local excision: The tumor and only part of the vulva, such as skin from the outer part or the inner part of the labia is removed. This might be done for small tumors on the surface of the skin.
- Skinning or superficial vulvectomy: This is rarely done. It removes only the top layer of skin that's affected by cancer.
- Simple partial vulvectomy: Most or all of the outer and inner labia, including the skin and the tissue just under the skin, is removed along with the tumor.
- Partial or modified radical vulvectomy: Part but not all of the vulva, along with deeper tissue under the skin, is removed.
- Simple vulvectomy: All of the vulva is removed, along with some of the tissue just under the skin.
- Complete or total radical vulvectomy: This surgery is rarely done. It removes all of the vulva, including the clitoris, and the deeper tissue under the skin. It may include parts of the inside of the upper thighs, lower belly, and the area between the vagina and anus (perineum). Lymph nodes in the groin are often removed too.
Talk with your healthcare provider about the type of surgery you will have. Be sure you understand exactly what will be done and what you can expect afterward. Know how your body will look, feel, and work after the vulvectomy. Don't be afraid to ask questions.
How to say it
vuhl-VEK-tuh-mee
Why vulvectomy is done
The surgery may be done to treat conditions such as:
-
Cancer of the vulva
-
Precancer of the vulva (called VIN, or vulvar intraepithelial neoplasia)
-
Skin cancer (melanoma) on the vulva
-
Severe skin disease, such as lichen sclerosus
-
Severe disease of sweat glands in the groin or vulva (hidradenitis suppurativa)
How vulvectomy is done
This is a general outline of what happens during vulva surgery:
-
You lie on an operating table. You're given medicine to make you sleep and not feel pain (general anesthesia) through the surgery. Or You may be given a shot into your lower back (spinal anesthesia) to make you numb from the waist down.
- A thin, soft tube (called a Foley catheter) is put in your urethra. This is to drain urine from your bladder during and after surgery.
-
The surgeon cleans the vulva and cuts away the diseased tissue. A small amount of healthy tissue around the tumor is also removed. This is to help make sure all the cancer is gone.
-
The surgeon will bring together edges of the skin and close them with stitches (sutures) or glue. Many times, small patches of healthy vulva skin are left and can build new tissue. In some cases, a skin graft is needed. This means a piece of healthy skin is taken from another part of your body. The skin graft is then stitched in place over the parts of the vulva that need to be covered.
-
The surgeon covers the area with a dressing to protect it and help it heal. If a skin graft was done, the spot the skin was taken from (the donor site) will also be covered.
-
The Foley catheter will likely stay in for as long as 2 weeks. It drains urine from your bladder while you heal.
You will need to stay in the hospital for a while after surgery. Again, your healthcare team can tell you what to expect.
After vulvectomy
Your healthcare team will watch you closely while you recover in the hospital. You may need bed rest for a period of time. Your provider will tell you when it's OK to sit up. When you're ready, they'll teach you what to do at home.
While you heal from the surgery, you may not be able to do certain activities. You may be told not to climb stairs and to limit your walking. You may also need to keep your legs close together. This is to help the incisions heal. You'll likely be told not to have sex for several weeks after surgery.
You'll be given pain medicine and stool softeners to help make it easy for you to have a bowel movement. You'll learn how to take care of any drains that must stay in as you heal and what kind of problems you should watch for. You'll also get instructions on how to keep your vulvar area clean. You may be told to soak in warm water several times a day (sitz bath). You may need to wear loose fitting clothes and no underwear for a few weeks.
Be sure you understand what you can and can't do as you recover from surgery. Rest when you are tired. Fatigue and weakness are normal for a few weeks. This will get better over time.
Risks of vulvectomy
-
Wound infection
- Problems with wound healing
- Urinary tract infection
-
Scarring
-
Changes in sexual function and body image
-
Need for more surgery to remove more tissue
-
Blood clots from bed rest
-
Excess bleeding
-
Incontinence or loss of control of the bladder or rectum
- Spraying of urine from scar tissue around the urethra
-
Blood blister under the skin (called a hematoma)
- Swelling in your groin or legs (called lymphedema)
Your healthcare provider will talk with you about when to seek medical attention. You may be told to call if you have any of the below:
- New symptoms or symptoms that get worse
- Signs of an infection such as a fever, odor, redness, or drainage
- Side effects that affect your daily function or don’t get better with treatment, such as pain or constipation
Ask your healthcare provider what signs to watch for and when to call. Know how to get help after office hours and on weekends and holidays.