Understanding Type 1 Diabetes
Your body breaks down food into sugar to get energy. When you have diabetes, your body has trouble using this sugar for energy.
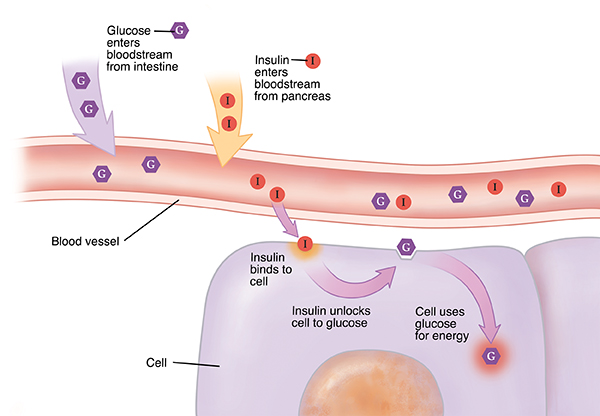
How the body normally gets energy
The digestive system breaks down food. This creates a sugar called glucose. Some of this sugar is stored in the liver. But most of it goes into your blood. It travels to your cells to be used as fuel. A hormone called insulin lets glucose go into the cells. Insulin is made in the pancreas. This is an organ in your belly. The insulin is released into the blood when there is glucose in the blood. Think of insulin as a key. Insulin attaches to the cell wall when it reaches a cell. This tells the cell to let glucose in.
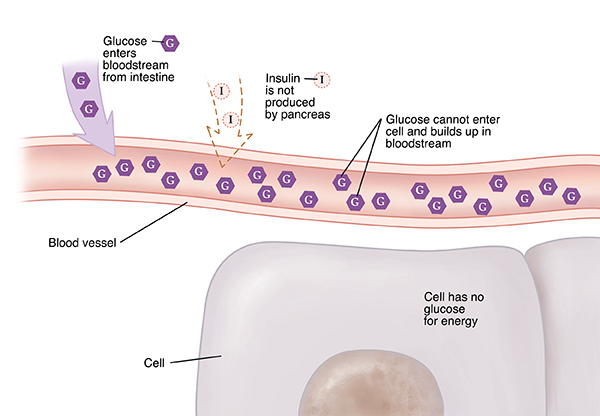
When you have type 1 diabetes
Special cells in the pancreas make insulin. These are called beta cells. In most people, type 1 diabetes is an autoimmune disease. This means the body's immune system harms the beta cells. Then the pancreas can't make as much insulin. In children, this often happens quickly. It isn't as fast in adults.
Some people have certain genes (traits passed on from parent to child) that make them more likely to develop type 1 diabetes. Diabetes occurs in these people when something sets off the immune system to start destroying the beta cells in the pancreas.
Diet and lifestyle habits don’t cause type 1 diabetes.
Glucose builds up
Without insulin, glucose can’t go into cells. It stays in your blood. Your liver puts even more glucose into the blood. This may lead to higher and higher blood sugar levels. This is called hyperglycemia. High blood sugar levels can cause serious health problems over time.
Ketones form
Your cells burn fat when they can’t get glucose to burn for energy. This leaves behind acids called ketones in your blood and urine. This is called ketosis. High blood sugar, high ketones, and other chemical changes in the blood (metabolic acidosis) can cause diabetic ketoacidosis (DKA). DKA is a dangerous condition. For some people, DKA is the first sign of type 1 diabetes.
Symptoms include:
Frequent urination.
Extreme fatigue.
Feeling thirsty.
Weight loss that is unexplained.
Fruity odor of the breath, difficulty breathing, vomiting, dizziness.
Diagnosis tools include:
Blood tests, to check for high blood sugar, ketones, and autoantibodies. The presence of autoantibodies indicates that your body is attacking itself. These are often found with type 1 diabetes but not with type 2 diabetes.
Urine tests, to check for ketones.
Insulin can be replaced
The insulin you are missing can be replaced. Insulin can't be taken by mouth. That's because it's broken down during digestion. But the insulin you are missing can be replaced with shots (injections) of insulin. Some people use an insulin pump. There are many different types of insulin sold in the United States, which differ in how they’re made, how they work in the body, and how much they cost. It’s also available in different strengths—most commonly, U-100.
Your doctor will help you find the right type of insulin for your health needs. With insulin being replaced, your body can burn glucose for energy. This helps keep your blood sugar in a healthy range.
Long-term complications
Over time, high blood sugar levels can harm blood vessels. This can lead to health problems. Keeping your blood sugar in a healthy range can help prevent or delay complications. Balancing insulin, diet, and activity is important. Complications may include:
Eye problems.
Kidney disease.
Nerve damage.
Digestion problems.
Sexual problems.
Tooth and gum problems.
Skin and foot problems.
Heart and blood vessel disease.
Your diabetes can be managed
Managing type 1 diabetes has both physical and emotional challenges. But you can do well by sticking to your medicine and glucose monitoring schedule. You can balance your medicine, your daily exercise, and your nutrition plan. Over time, these things will get easier to do.
Ask your care team about a service called diabetes self-management education and support. You will learn skills to help you better manage your diabetes and find support when you need it. This service may be given in a group setting or one-on-one with your care team. It may also be available via telehealth.