Having Pericardiocentesis
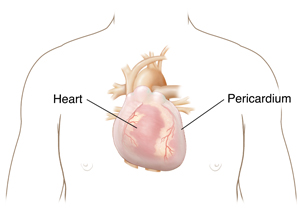
Pericardiocentesis is a procedure to remove fluid that has built up in the sac around the heart (pericardium). The fluid is drained with a needle and a thin, flexible tube (catheter).
What to tell your healthcare provider
Tell your healthcare provider about all the medicines you take. This includes over-the-counter medicines such as ibuprofen. It also includes vitamins, herbs, and other supplements, and any illegal drug use.
Tests before your procedure
You may need some tests before the procedure, such as:
-
Chest X-ray
-
Electrocardiogram (ECG), to check the heart rhythm
-
Blood tests, to check your overall health
-
Echocardiogram, to view blood flow through the heart and the fluid around the heart
-
CT scan or MRI, if the doctor needs more information about your heart
-
Heart catheterization, to look at the coronary blood vessels
Getting ready for your procedure
Talk with your healthcare provider how to get ready for your procedure. Follow your healthcare provider’s instructions about what medicines to stop taking before the procedure. Don’t stop taking any medicine unless your healthcare provider tells you to.
Make sure to do the following:
-
Arrange for a family member or friend to take you home from the hospital.
-
Follow any directions you're given for not eating or drinking before surgery.
-
Follow all other instructions from your healthcare provider.
You may be asked to sign a consent form that gives your permission to do the procedure. Read the form carefully. Ask questions if something is not clear.
On the day of your procedure
Your procedure will be done by a cardiologist. This is a doctor who specializes in diseases of the heart. They'll work with a team of specialized nurses. The procedure takes about 1 hour. It may take place in a cardiac catheterization lab. Ask your doctor about the details of your procedure. In general, you can expect the following during a catheter pericardiocentesis, the most common form:
-
An IV (intravenous) line will be put in your hand or arm. You'll likely be given medicine to make you sleepy during the procedure.
-
A healthcare provider will watch your vital signs, like your heart rate and blood pressure, during the procedure.
-
Your doctor will do an echocardiogram of the heart. This is a painless non-invasive imaging test that uses ultrasound waves to create an image of the inside of your body. It’s done to view the structure of your heart, and the fluid around the heart. This helps the doctor find the best place to insert the needle.
-
The doctor will put a local anesthetic on the needle insertion site, below the breastbone.
-
The doctor will insert the needle through the skin. You may feel this as pressure or slight pain. You can have pain medicine if needed.
-
The doctor will guide the needle to the fluid in the pericardial sac. They'll use an echocardiogram to help with this. Or the doctor may use live X-ray imaging called fluoroscopy.
-
Once the needle is in the right area, the doctor will put a catheter in that place. The needle will then be removed. Fluid will drain out through the catheter.
-
The doctor will remove the catheter when enough fluid has drained. The catheter may stay in place for several hours or days. Or it may be removed sooner. Pressure will be put on the catheter insertion site to prevent bleeding.
After your procedure
You will feel drowsy after the procedure. You will soon begin to feel more awake and aware. You'll be closely watched as you become more alert. You may need to stay in the hospital for one or more days. This may depend on the reason for your procedure.
A sample of the fluid from around your heart may be sent to a lab for testing. You may have a chest X-ray. This is to make sure the needle did not puncture your lung during the procedure.
When you go home, you should be able to go back to your normal activities. Don't do any vigorous exercise until your doctor says you are ready.
Follow-up care
Make sure you keep all of your follow-up appointments. Follow all the instructions your healthcare provider gives you for medicines, exercise, diet, and wound care.
When to call your healthcare provider
Call your healthcare provider right away if you have any of these:
-
Fever of 100.4°F (38°C) or higher, or as directed by your provider
-
Increase in fluid leaking from the needle insertion site
-
Chest pain
-
Other symptoms as advised