Having Minimally Invasive Total Knee Replacement
Total knee replacement is a type of surgery to replace a damaged knee joint. Minimally invasive surgery uses two or more small cuts (incisions) instead of one large incision. The procedure is done by an orthopedic surgeon. This is a healthcare provider with special training in treating bone, joint, and muscle problems.
What to tell your healthcare provider
Tell your healthcare provider about all the medicines you take. This includes over-the-counter medicines such as ibuprofen. It also includes vitamins, herbs, other supplements, and any illegal drugs. And tell your healthcare provider if you:
-
Have had any recent changes in your health, such as an infection or fever
-
Are sensitive or allergic to any medicines, latex, tape, or anesthesia (local and general)
-
Are pregnant or think you may be pregnant
Tests before your surgery
Before your surgery, you may need imaging tests. These may include ultrasound, X-rays, CT scan, or MRI.
Getting ready for your surgery
Talk with your surgeon about how to get ready for your surgery. You may need to stop taking some medicines before the procedure, such as blood thinners and aspirin. If you smoke, you may need to stop before your surgery. Smoking can delay healing. Talk with your healthcare provider if you need help to stop smoking.
Also, make sure to:
-
Ask a family member or friend to take you home from the hospital
-
Follow any directions you are given for not eating or drinking before surgery
-
Follow all other instructions from your healthcare provider
You will be asked to sign a consent form that gives your permission to do the procedure. Read the form carefully. Ask questions if something is not clear.
Planning for recovery
You will also need to plan some changes at home to help you recover. Talk with your surgeon about how you need to prepare for your recovery. You may need to:
-
Go to a rehabilitation facility or have rehab at home
-
Get extra help at home with bathing and dressing, meals, or shopping
-
Make changes to your home to prevent falls and make your recovery easier, such as a raised toilet seat, grab bars, or handrails
On the day of your surgery
Your orthopedic surgeon will work with a team of specialized nurses. This surgery may be done using a few small incisions. Ask your healthcare provider about the details of your surgery. The whole procedure may take a couple of hours. In general you can expect the following:
-
You may have general anesthesia, a medicine that allows you to sleep through the surgery. You won’t feel any pain during the surgery. Or you may have medicine to numb the area (regional anesthesia) and medicine to help you relax and sleep (sedation) through the surgery.
-
A healthcare provider will watch your heart rate, blood pressure, and other vital signs during the surgery.
-
You may be given antibiotics during and after the surgery. This is to help prevent infection.
-
After cleaning the skin, the surgeon makes a cut (incision) through the skin and muscles near the knee.
-
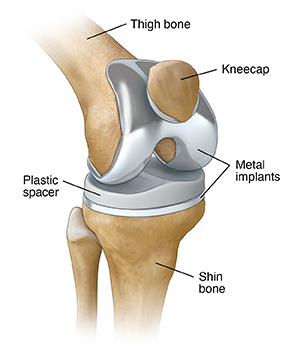
The surgeon removes the damaged portions of your thigh and shin bones. They also remove a small amount of healthy bone under the damaged bone.
-
The surgeon puts metal implants into the joint space. They are cemented to the remaining bone.
-
The surgeon may also remove part of the underside of the kneecap.
-
The surgeon puts a plastic spacer between the metal implants. This will let you move your knee more easily.
-
The surgeon closes the layers of muscle and skin with stitches (sutures), staples, or other means.
After your surgery
Talk with your surgeon about what you can expect after your surgery. In the hospital, you will probably have physical therapy and may use a continuous passive motion exercise machine. You may be able to leave the hospital 1 to 2 days after surgery. Or you may be able to leave the same day. Before leaving the hospital, you will likely have X-rays taken of your knee. This is to check the surgery.
Recovering at home
You will have some pain after the surgery. Your surgeon will tell you what pain medicine you can take to help reduce the pain. You can also use ice packs to help lessen pain and swelling. You might have some fluid draining from your incisions. This is normal.
You will get instructions about how you can move your knee and leg. You may need to use crutches, a cane, or walker for a few days or weeks.
Follow all of your healthcare provider's instructions carefully. Your surgeon may tell you to:
-
Take prescription medicine to prevent blood clots
-
Not take certain over-the-counter medicines for pain that may interfere with bone healing
-
Eat foods high in calcium and vitamin D to help with bone healing
Follow-up care
Make sure to keep all of your follow-up appointments. You may need to have your stitches or staples removed a week or so after your surgery.
You may have physical therapy. This is to improve the strength and movement of your leg. The therapy may include treatments and exercises. The therapy improves your chances of a full recovery. Most people are able to return to light activities within a couple of weeks of the surgery. After your surgery, you should have less pain. But you may still have a stiff knee joint.
You may need another knee surgery 10 to 20 years after your first knee replacement. You can help delay when you will need a follow-up surgery by:
-
Doing regular low-impact exercise such as walking
-
Not doing high-impact exercise such as jogging
-
Preventing falls
When to call your healthcare provider
Call your healthcare provider right away if you have any of these:
-
Fever of 100.4°F (38.0°C) or higher, as directed by your healthcare provider
-
Shaking chills
-
Redness, bad smell, or fluid leaking from your incision that gets worse
-
Pain in your knee or leg that gets worse
-
Calf pain and progressive swelling