Having Minimally Invasive Total Hip Replacement
Total hip replacement is a type of surgery to replace a damaged hip joint. Minimally invasive surgery uses 1 or more small cuts (incisions) instead of 1 large cut. The procedure is done by an orthopedic surgeon. This is a healthcare provider with extra training in treating bone, joint, and muscle problems.
What to tell your healthcare provider
Tell your healthcare provider about all the medicines you take. This includes:
- Over-the-counter medicines, such as ibuprofen
- Vitamins
- Herbs
- Other supplements
And tell your provider if you:
-
Have had any recent changes in your health, such as an infection or fever
-
Are sensitive or allergic to any medicines, latex, tape, or local or general anesthesia
-
Are pregnant or think you may be
Tests before your surgery
Before your surgery, you may need imaging tests. These may include ultrasound, X-rays, CT scan, or MRI.
Getting ready for your surgery
Talk with your healthcare provider about how to get ready for your surgery. You may need to stop taking medicines. These include blood thinners and aspirin before the procedure. If you smoke, stop before your surgery. Smoking can delay healing. Talk with your provider if you need help to stop smoking.
Also make sure to:
-
Ask a family member or friend to take you home from the hospital
-
Follow all directions you are given for not eating or drinking before surgery
-
Follow all other instructions from your provider
You will be asked to sign a consent form. This gives your provider permission to do the procedure. Read the form carefully. Ask questions if you have concerns or something is not clear.
Planning for recovery
You will also need to plan some changes at home to help you recover. Talk with your provider about what to expect. You may need to:
-
Go to a rehab facility or have rehab at home
-
Get extra help at home with bathing and dressing, meals, or shopping
-
Make changes to your home to prevent falls and make your recovery easier. This may be a raised toilet seat, grab bars, or handrails.
On the day of your surgery
Your orthopedic surgeon will work with a team of nurses and staff. This surgery may be done using a few small incisions. Ask your surgeon about the details of your surgery. The surgery may take a few hours. In general, here is what you can expect:
-
You may have general anesthesia. This is a medicine that lets you comfortably sleep through the surgery. You will not be awake or feel any pain. Another choice is medicine to numb the area (regional anesthesia). This is given along with medicine to help you relax and sleep (sedation).
-
A healthcare provider will watch your heart rate, breathing, oxygen level, and blood pressure during the surgery.
-
You may be given antibiotics during and after the surgery. This is to help prevent infection.
-
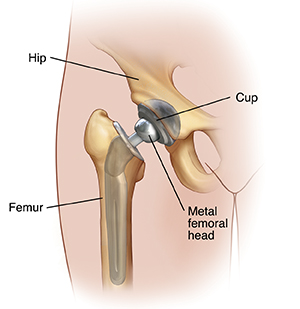
After cleaning the skin, the surgeon makes 1 or 2 small incisions through the skin and muscles near the hip.
-
The surgeon takes the femoral head out of the joint socket.
-
They replace the femoral head with a metal one.
-
The surgeon then removes the damaged cartilage and bone from the joint socket.
-
They put a metal cup into the socket. Screws may be used to hold it in place.
-
The surgeon places the femoral head back in the socket.
-
They then close the layers of muscle and skin with stitches or staples.
After your surgery
Talk with your surgeon about what you can expect after your surgery. You may be able to leave the hospital the same day. Or you may spend 1 to 3 days in the hospital after surgery. Before leaving the hospital, you will likely have X-rays taken of your hip. This is to check the surgery.
Recovering at home
You will likely have some pain after the surgery. Your healthcare provider will tell you what pain medicine you can take. You can also use ice packs to help ease pain and swelling. You might have some fluid draining from your incisions. This is normal.
You will get instructions about how you can move your hip and leg. You may need to use crutches, a cane, or walker for a few days or weeks.
Follow all your provider’s instructions. Your surgeon may tell you to:
-
Take prescription medicine to prevent blood clots
-
Not take some medicines for pain that may delay bone healing
-
Eat foods high in calcium and vitamin D to help with bone healing
Follow-up care
Make sure to keep all your follow-up appointments. You may need to have your stitches or staples removed 1 week or so after your surgery.
You will be prescribed physical therapy. This is to improve the strength and movement of your leg. It improves your chances of a full recovery. The therapy may include treatments and exercises. You will likely be able to return to light activities within 2 weeks of the surgery.
You may need another hip surgery 10 to 20 years after your first surgery. You can help delay the follow-up surgery by doing regular exercise and preventing falls.
Call 911
Call 911 right away if you have either of these:
-
Chest pain
-
Shortness of breath
When to call your healthcare provider
Call your healthcare provider right away if you have any of these:
- Hip pain that gets worse
- Pain, swelling, or redness in your calf or leg not near your incision
- Fever of 100.4°F (38°C) or higher, or as advised by your provider
- Chills
- Swelling or redness at the incision site that gets worse
- Fluid leaking or bad smell from the incision