How does ECMO work?
Blood is removed from the patient through a cannula and routed through a pump and oxygenator which efficiently removes carbon dioxide and oxygenates the blood. The blood is then returned to the patient through the same or a separate cannula at flows up to seven liters per minute. ECMO minimizes or eliminates the need for ventilator and cardiovascular support allowing for organ rest and recovery. Without the use of ECMO the extremes of patient management such as excessive ventilator settings, inotropes, and vasopressors, can create ongoing organ injury and further harm.
Are there risks associated with ECMO?
Risks include bleeding, thromboembolism, leg ischemia, stroke, infection, and device-related complications.
How long can I expect my patient to need ECMO support?
It depends, but organ recovery usually occurs in a week or two. Occasionally, patients may need to be supported for a longer time.
What is the difference between veno-venous (VV) and veno-arterial (VA) ECMO?
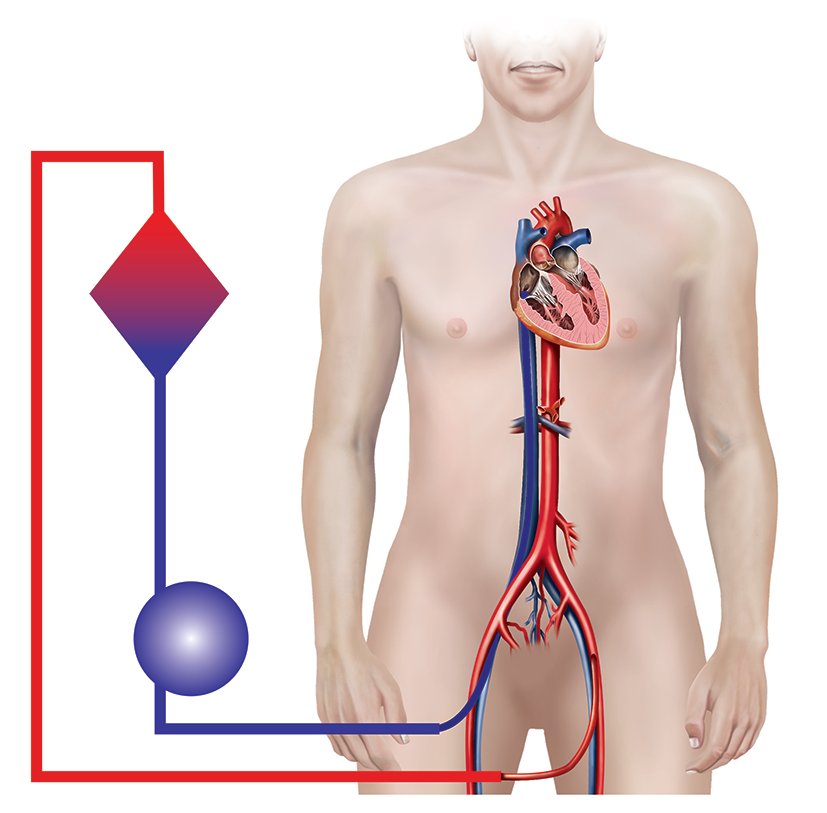
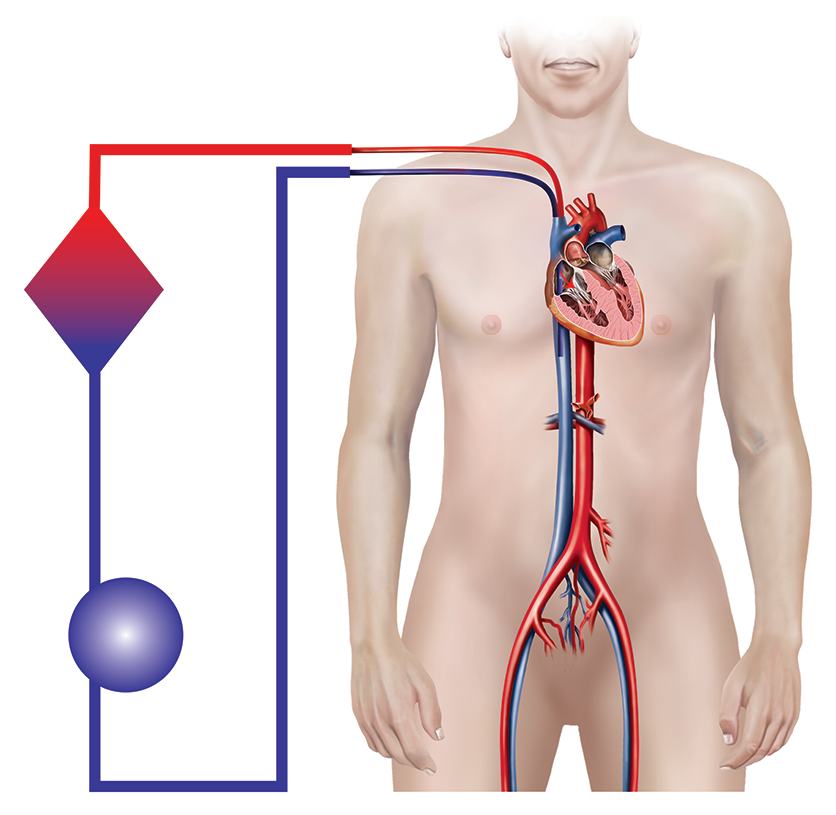
Two types of ECMO are available for use. Veno-Venous (VV) ECMO is used for severe respiratory failure and in most cases is accomplished through a single cannula placed into the internal jugular vein. Veno-Arterial (VA) ECMO is used for severe cardiac failure, including cardiac arrest, and is usually done with cannulation of the femoral artery and vein.
Veno-arterial (VA):
Veno-venous (VV):