Skin Cancer
The risk posed by a skin cancer diagnosis can range from mild to life-threatening. We have the expertise you need to protect, prevent, or treat against skin cancer. Our specialists use the most advanced methods to accurately diagnose skin cancer and the most innovative therapies needed to treat it.
Types of Skin Cancer
Skin cancer is a serious disease that can affect anyone at any age. It's the most common kind of cancer in the U.S. If found early, when it's small and hasn't spread, some of the more common types of skin cancer can often be cured. But some types of skin cancer can be life-threatening.
Talk with your healthcare provider about what you can do to help prevent skin cancer. Ask about regular skin exams as part of your routine physicals. You can also ask about doing monthly self-exams of your skin. If you see any changes in your skin, see your healthcare provider right away.
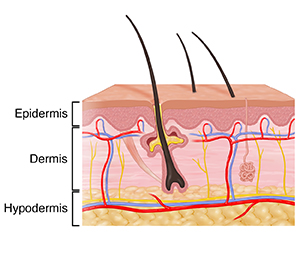
Understanding the skin
The skin is made up of three layers: epidermis, dermis, and hypodermis:
Epidermis. This is the thin outer layer of the skin. The epidermis is made of multiple layers. It's the main barrier to the world outside our bodies. It's made primarily of two types of cells: keratinocytes and melanocytes.
- Keratinocytes are the most common type of cells in the epidermis. They are the structural cells of the epidermis. They are sometimes divided into several groups:
- Basal cells are round cells found at the inner base layer of the epidermis. These divide to replace lost skin cells. As new skin cells are formed, they flatten and move closer to the surface of the skin.
Squamous cells are flat cells in the outermost layer of the epidermis. They are always shedding off as new ones are forming.
- Melanocytesare scattered through the basal layer. They make melanin to give skin its color.
- Keratinocytes are the most common type of cells in the epidermis. They are the structural cells of the epidermis. They are sometimes divided into several groups:
- Dermis.This middle layer of skin is where blood and lymph vessels, hair follicles, oil and sweat glands, nerves, and collagen are found. It supports the epidermis and is a key part of wound healing. It also gives the skin flexibility and strength.
- Hypodermis.This is the deepest layer of the skin. It's made of fat, collagen, and blood vessels. It helps insulate the body and absorb shock, and it protects the body from injury.
Most skin cancer forms in the epidermis. It usually starts in the keratinocytes or melanocytes.
Skin cancer can be grouped into two types: non-melanoma (also called keratinocyte carcinomas) and melanoma.
The two most common types of non-melanoma skin cancer are basal cell carcinoma and squamous cell carcinoma.
Basal cell cancer
Basal cell cancer is the most common type of skin cancer. It is derived from young keratinocytes, and under the microscope looks most like the round basal cells seen at the base of the epidermis. It's usually found on sun-exposed skin, like the face, ears, neck, trunk, or arms, but it can start anywhere.
These lesions vary in color and may be waxy, pearly, scaly, or scar-like. Tiny blood vessels can sometimes be seen through the lesion’s surface. These lesions can bleed easily and might not heal well. Nearly all basal cell cancers can be treated and cured if they're found early.
Squamous cell cancer
Squamous cell cancer is the second most common type of skin cancer. It is also derived from young keratinocytes, but under the microscope looks more like flat squamous cells. Lesions often form on the face, ears, neck, hands, or arms—places that get a lot of sun. The lesions are firm, red bumps or flat, scaly, crusty growths. They may be sores that keep healing and reopening.
Squamous cell carcinoma is more likely to grow and spread to other parts of the body than basal cell carcinoma, though this is rare. Most squamous cell carcinoma is found early enough to be treated and cured.
Melanoma
Melanoma is a less common but much more dangerous kind of skin cancer. It starts in skin cells called melanocytes. It's much more likely to grow and spread than basal or squamous cell cancers. Finding and treating it early is key.
It's often not easy to tell where a melanoma lesion’s borders are. It's often brown or black but may be a mix of colors with pink, tan, or white. The shape and size of melanoma lesions tend to differ from one side to the other. Melanoma is most often found on sun-exposed skin, but it can start anywhere, like the genitals, mouth, palms of hands, bottoms of feet, under the nails, and even in your eyes.
Less common skin cancers
There are other serious types of non-melanoma skin cancer, too. These include Merkel cell cancer, Kaposi sarcoma, and skin (cutaneous) lymphomas, but these cancers are very rare.
Actinic keratosis
Actinic keratosis (AK) is not skin cancer. AK develops when there is damage to keratinocytes, most often caused by too much sun exposure. It's a common, pre-cancer skin change that can turn into a squamous cell skin cancer over time if it's not treated. Most AK doesn't turn into cancer, but it's important to have any skin changes looked at by a healthcare provider.
AK lesions tend to be found on sun-exposed parts of the body. They can be pink, reddish-brown, or skin-colored. These lesions are often small, raised, scaly, and rough, like sandpaper. In some cases, AK lesions hurt. Most people with them have more than one lesion. Getting early treatment for AK almost always cures the lesions.
What is melanoma?
Cancer starts when cells change and grow out of control. The changed (abnormal) cells often grow to form a lump or mass called a tumor. Cancer cells can also grow into (invade) nearby areas. And they can spread to other parts of the body. This is called metastasis.
Melanoma is a serious type of skin cancer. It starts in skin cells called melanocytes. These are cells that give skin its color. Melanoma is much less common than other types of skin cancer that start in other skin cells. But it's more likely to spread to other parts of the body.
Melanoma can happen anywhere on the skin. It's most often found in areas exposed to the sun. Men usually get it between the shoulders and the hips. They may also get it on their head or neck. Women usually get it on their arms and lower legs. Sometimes melanoma starts in skin that's never exposed to sunlight, like the mouth, genitals, and anus. It may even start in the eye, under a fingernail or toenail, and in the nose and sinuses.
Who is at risk for melanoma?
A risk factor is anything that may increase your chance of having a disease. The exact cause of someone’s cancer may not be known. But risk factors can make it more likely for a person to have cancer. Some risk factors may not be in your control. But others may be things you can change.
The most common risk factors for melanoma include:
- Greater amount of time spent in the sun
- Use of tanning booths or beds and sunlamps
- Many moles or abnormal ones
- Fair skin, blue eyes, freckles, or light hair
- Family history of melanoma
- Certain inherited gene changes and conditions, like xeroderma pigmentosum, Li-Fraumeni syndrome, and hereditary breast and ovarian cancer syndromes
- Past history of skin cancer (any kind)
- Weakened immune system
Talk with your healthcare provider about your risk factors for melanoma and what you can do about them.
Can melanoma be prevented?
There is no sure way to prevent melanoma, but there are things you can do that may help lower your risk for it, such as:
- Wearing broad-spectrum sunscreen with SPF 30 or higher
- Not using tanning booths or beds and sunlamps
- Practicing sun safety. Limit time in the sun when UV light is strongest – between 10 a.m. and 4 p.m.
- Wearing sunglasses that have 100% UVA/UVB protection
- Wearing clothing to shade your face and cover your body
- Doing skin checkups often
Regular skin self-exams may help you find skin cancer early, when it’s smaller and easier to treat. Become familiar with the way your skin and moles look. Talk with your healthcare provider about any changes, including bumps, spots, or other marks on your skin.
What are the symptoms of melanoma?
The first symptom of melanoma is often a change in a mole or the appearance of a new mole. The ABCDE rule can help you tell a normal mole from one that might be melanoma. The rule is:
- Asymmetry. One half of the mole does not match the other half.
- Border irregularity. The edges of the mole are ragged or irregular.
- Color. The mole has different colors in it. It may be tan, brown, black, red, or other colors. Or it may have areas that appear to have lost color.
- Diameter. The mole is bigger than 6 mm or ¼ inch across, about the size of a pencil eraser. But some melanomas can be smaller.
- Evolving. A mole changes in size, shape, or color.
Other symptoms that may be melanoma include:
- A mole that hurts, itches, or is sore
- A mole that oozes, bleeds, or becomes crusty
- A mole that looks different from your other moles
- A sore that doesn't heal
- A mole or sore that becomes red or swells at its edges or beyond
Many of these may be caused by other health problems. Still, it's important to see a healthcare provider if you have these symptoms. Only a healthcare provider can tell if you have cancer.
How is melanoma diagnosed?
If your healthcare provider thinks you may have melanoma, you'll need certain exams and tests. You'll be asked about your health history, your symptoms, risk factors, and family history of disease. A physical exam and skin exam will be done. You may also have a biopsy.
A biopsy is the only way to confirm cancer. Tiny pieces of the changed mole or skin are removed and sent to a lab. Then they're tested for cancer cells. Ask you healthcare team when you will get your results.
After a diagnosis of melanoma, you'll need more tests. These help your healthcare providers learn more about your overall health and the cancer. They're used to find out the stage of the cancer. The stage is how much cancer there is and how far it has spread (metastasized) in your body. It's one of the most important things to know when deciding how to treat the cancer.
Once your cancer is staged, your provider will talk with you about what the stage means for your treatment. Be sure to ask your provider to explain the details of your cancer to you in a way you can understand.
How is melanoma treated?
Your treatment choices depend on the size, place, and stage of your melanoma. The goal of treatment may be to cure you, control the cancer, or help ease problems caused by cancer. Talk with your healthcare team about your treatment choices, the goals of treatment, and what the risks and side effects may be. Other things to think about are if the cancer can be removed with surgery, how your body will look after treatment, and your overall health.
Types of treatment for cancer are either local or systemic. Local treatments remove, destroy, or control cancer cells in one area. Surgery and radiation are local treatments. Surgery is the most common way to treat melanoma. Systemic treatment is used to destroy or control cancer cells that may have traveled around your body. When taken by pill or injection, chemotherapy and targeted therapy are systemic treatments. You get just one treatment or a combination of treatments.
Melanoma may be treated with:
- Surgery
- Radiation therapy
- Chemotherapy
- Immunotherapy
- Targeted therapy
Talk about your concerns with your provider before making a decision.
What are treatment side effects?
Surgery to remove your melanoma will always result in a scar. Talk with your healthcare provider about the size and type of scar you may end up with.
Cancer treatment, such as chemotherapy and radiation, can damage normal cells. This can cause side effects like hair loss, mouth sores, and vomiting.
Talk with your provider about side effects linked with your treatment. There are often ways to manage them. There may be things you can do and medicines you can take to help prevent or control many treatment side effects.
Coping with melanoma
Many people feel worried, depressed, and stressed when dealing with cancer. Getting treatment for cancer can be tough on the mind and body. Keep talking with your healthcare team about any problems or concerns you may have. Work together to ease the effect of cancer and its symptoms on your daily life.
Here are tips:
- Talk with your family or friends.
- Ask your healthcare team or social worker for help.
- Speak with a counselor.
- Talk with a spiritual advisor, such as a minister or rabbi.
- Ask your healthcare team about medicines for depression or anxiety.
- Keep socially active.
- Join a cancer support group in person or online.
Cancer treatment is also hard on the body. To help yourself stay healthier, try to:
- Eat a healthy diet with as many protein foods as possible.
- Drink plenty of water, fruit juices, and other liquids.
- Keep physically active.
- Rest as much as needed.
- Talk with your healthcare team about ways to manage treatment side effects.
- Take your medicines as directed by your team.
When should I call my healthcare provider?
Your healthcare provider will talk with you about when to call. You may be told to call if you have any of the following:
- New symptoms or symptoms that get worse
- Signs of an infection, such as a fever
- Side effects of treatment that affect your daily function or don’t get better with treatment
Ask your provider what signs to watch for and when to call. Know how to get help after office hours and on weekends and holidays.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your healthcare provider if you have questions, especially after office hours or on weekends.
What is nonmelanoma skin cancer?
Cancer is made of changed cells that grow out of control. The changed (abnormal) cells often grow to form a lump or mass called a tumor. Cancer cells can also grow into (invade) nearby areas. And they can spread to other parts of the body. This is called metastasis.
Skin cancer is a disease that begins in the cells of the skin. Nonmelanoma skin cancer is the most common type of cancer in the U.S. The most common type of nonmelanoma skin cancers are called keratinocyte cancers. These cancers have 2 main types called basal cell skin cancer and squamous cell skin cancer. Basal cell skin cancer is much more common than squamous cell skin cancer. Both types are most often caused by ultraviolet (UV) light from the sun damage over time.
There are other less common types of nonmelanoma skin cancer. These include:
- Merkel cell carcinoma
- Cutaneous T-cell lymphoma
- Kaposi sarcoma
Who is at risk for nonmelanoma skin cancer?
A risk factor is anything that may increase your chance of having a disease. The exact cause of someone’s cancer may not be known. But risk factors can make it more likely for a person to have cancer. Some risk factors may not be in your control. But others may be things you can change.
The most common risk factors for nonmelanoma skin cancer include:
- Greater amount of time spent in the sun
- The use of tanning beds, booths and sunlamps
- Certain features, such as fair skin, light hair (red or blond), and light eyes (green, blue, or gray)
- Lots of freckles and skin burns easily in the sun
- Personal history of skin cancer or pre-cancer
- Older age
- Being a man
- Weakened immune system
- Exposure to large amounts of arsenic
- Past radiation treatment
- Scars, burns, or inflamed skin
- Smoking
- HPV (human papillomavirus) infection
- Certain rare inherited conditions, such as xeroderma pigmentosum
- Medicines that can increase skin sensitivity to sunburns
Talk with your healthcare provider about your risk factors for nonmelanoma skin cancer and what you can do about them.
Can nonmelanoma skin cancer be prevented?
There is no sure way to prevent nonmelanoma skin cancer. But there are some things that may help lower your risk for it, such as:
- Wearing sunscreen with an SPF of 30 or higher
- Not using tanning beds, booths or sunlamps
- Limiting your sun exposure when UV (ultraviolet) light is strongest, between 10 a.m. and 4 p.m.
- Wearing sunglasses (100% UVA/UVB protection)
- Wearing clothing to shade your face, neck, and cover your body
- Doing skin checks
- Treating skin pre-cancers early
You may be able to spot skin cancer early when it’s easier to treat by doing a regular skin self-exam. If you are at risk, see a dermatologist regularly. That may also allow you to detect skin cancers when they're easier to treat. Become familiar with the way your skin and moles look. Talk with your healthcare provider about any bumps, spots, or other marks that appear on your skin. Show your provider any area of skin that doesn’t look normal.
What are the symptoms of nonmelanoma skin cancer?
Nonmelanoma skin cancer often develops in areas exposed to the sun, such as the head, face, neck, rim of your ear, arms, hands, trunk of your body (chest, abdomen, and back), and legs. But it can start anywhere on the body. It may appear as a new growth. Or it may occur as a change in the size or in the color of a growth you already have. These changes can happen slowly or quickly.
Here are some possible signs of the most common nonmelanoma skin cancers:
- A small, raised bump that is shiny or pearly
- A small, flat spot that is scaly, irregularly shaped, and pale, pink, or red
- Sores that don't heal
- A growth with raised edges, a lower area in the center, and brown, blue, or black areas
- A wart-like growth that might bleed or crust over
- Scaly patches or bumps that are often red or purple and itch
Many of these may be caused by other health problems. But it is important to see a healthcare provider if you have these symptoms. Only a healthcare provider can tell if you have cancer.
How is nonmelanoma skin cancer diagnosed?
Diagnosing skin cancer starts with checking out a bump, spot, or other mark on your skin. If your healthcare provider thinks you may have nonmelanoma skin cancer, you will need certain exams and tests. Your healthcare provider may ask you to see a skin specialist provider called a dermatologist. Your healthcare provider will ask you about your health history, your symptoms, risk factors, and family history of disease. They will also give you a physical exam. You will likely have a biopsy.
A biopsy is the only way to confirm cancer. Small pieces of tissue are taken out and checked in a lab for cancer cells. Your results will come back in about 1 week.
If your healthcare provider is concerned that your skin cancer is more aggressive, you may have other tests. These help your healthcare providers learn more about the cancer. They can help determine the stage of the cancer. The stage is how much and how far the cancer has spread (metastasized) in your body. It's one of the most important things to know when deciding how to treat the cancer.
Once your cancer is staged, your healthcare provider will talk with you about what the stage means for your treatment. Ask your provider to explain the stage of your cancer to you in a way you can understand.
How is nonmelanoma skin cancer treated?
Your treatment choices depend on the type of nonmelanoma skin cancer, how large the skin cancer is, where it is, and what stage it is. It also depends on the test results. The goal of treatment may be to cure you, control the cancer, or help ease problems caused by the cancer. Talk with your healthcare team about your treatment choices, the goal of treatment, and the possible risks and side effects. Other things to think about are if the cancer can be removed with surgery and your overall health.
Types of treatment for cancer are either local or systemic. Local treatments remove, destroy, or control cancer cells in one area. Systemic treatment is used to destroy or control cancer cells that may have traveled through your body. Surgery and radiation are local treatments. When taken by pill or injection, chemotherapy is a systemic treatment. You may have one or a combination of treatments.
Nonmelanoma skin cancer may be treated with:
- Surgery
- Creams applied to the affected area
- Chemotherapy
- Targeted therapy
- Radiation therapy
- Photodynamic therapy
- Immunotherapy
Talk with your healthcare providers about your treatment options. Make a list of questions. Think about the benefits and possible side effects of each option. Talk about your concerns with your healthcare provider before making a decision.
What are the treatment side effects?
Cancer treatment such as radiation therapy can damage normal cells. This can cause side effects like red, dry, burning skin in the area being treated, risk of infection, and hair loss and rash in the treatment area.
Surgery is the most common way to treat nonmelanoma skin cancer. There are many methods of surgery that can be used to remove the cancer. Side effects from surgical procedures depend upon the type of procedure. They may include bruising, risk of infection, scarring, pain, redness, or swelling at the site.
Talk with your healthcare provider about side effects you might have and ways to manage them. There may be things you can do and medicines you can take to help prevent or control side effects.
Coping with nonmelanoma skin cancer
Most nonmelanoma cancers are not life-threatening and can be treated by a dermatologist. However, people may worry or feel stressed when dealing with nonmelanoma cancer. Getting treatment for cancer can be tough on the mind and body. Keep talking with your healthcare team about any problems or concerns you have. Work together to ease the effect of cancer and its symptoms on your daily life.
Here are some tips:
- Talk with your family or friends.
- Ask your healthcare team or social worker for help.
- Speak with a counselor.
- Talk with a spiritual advisor, such as a minister or rabbi.
- Ask your healthcare team about medicines for depression or anxiety.
- Keep socially active.
- Join a cancer support group.
Cancer treatment is also hard on the body. To help yourself stay healthier, try to:
- Eat a healthy diet, with a focus on high-protein foods.
- Drink plenty of water, fruit juices, and other liquids.
- Keep physically active.
- Rest as much as needed.
- Talk with your healthcare team about ways to manage treatment side effects.
- Take your medicines as directed by your team.
When should I call my healthcare provider?
Your healthcare provider will talk with you about when to call. You may be told to call if you have any of the below:
- New symptoms or symptoms that get worse
- Signs of an infection, such as a fever
- Side effects of treatment that affect your daily function or don’t get better with treatment
Ask your healthcare provider what signs to watch for and when to call. Know how to get help after office hours and on weekends and holidays.
Next steps
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions, especially after office hours and on weekends and holidays.