Cardiovascular Disease Fellowship Rotations
Rotations
The program offers great flexibility and can be tailored to meet the fellows' interests and career goals. During their training, fellows experience a balanced schedule including:
- Core clinical rotations in cardiac intensive care, inpatient consultative cardiology, clinical electrophysiology, and advanced heart failure
- Laboratory-based rotations in imaging and noninvasive laboratories as well as the cardiac catheterization and electrophysiology laboratories
- Research rotations
- Twelve elective rotations, including 11 electives during the third year of training
- Volume and breadth of training that allows for specialization in one or more modalities as defined by COCATS 4
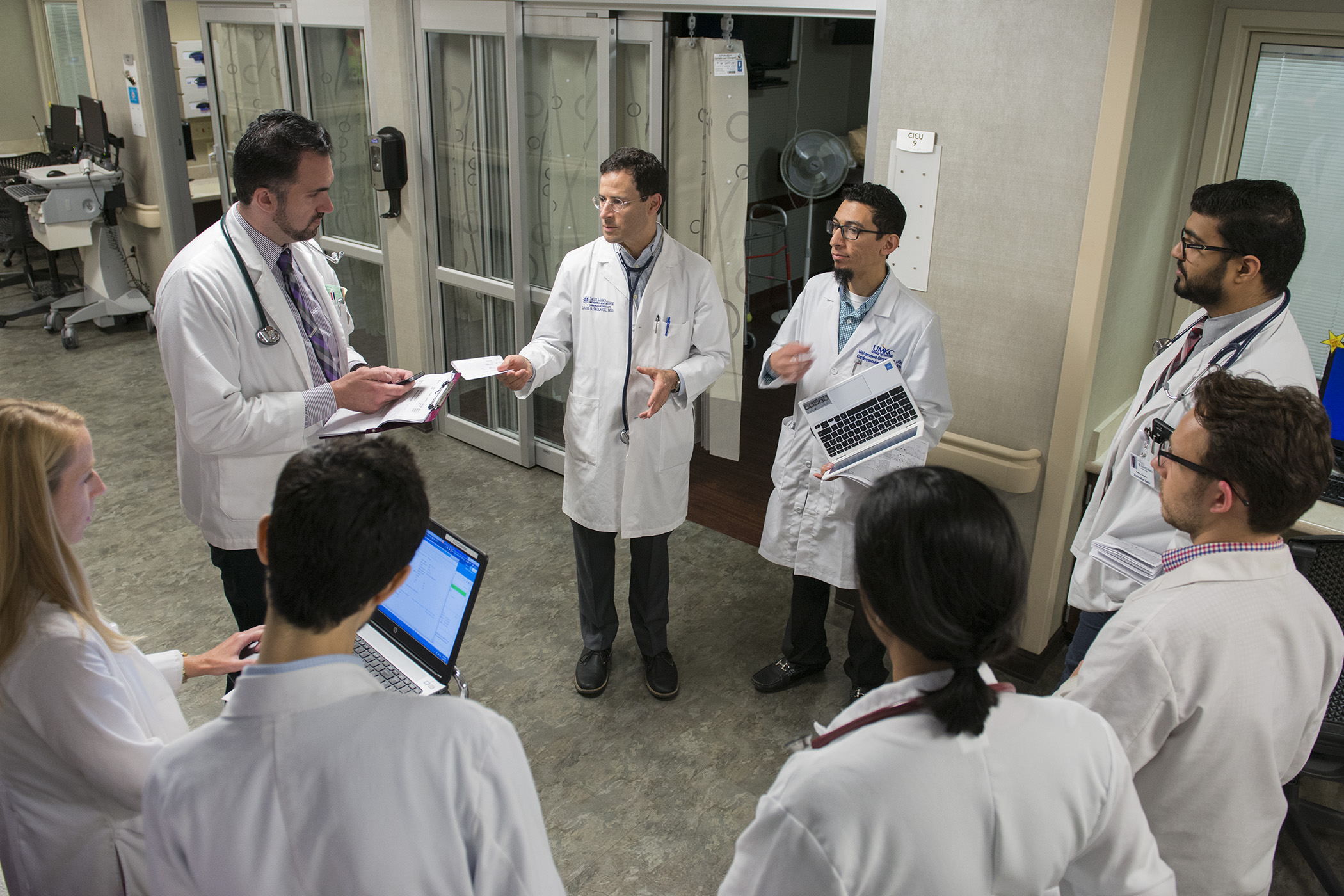
Cardiac Intensive Care Unit and clinical consultative cardiology
During the first and second years of training, fellows round in both the Cardiac Intensive Care Unit (CICU) and on the inpatient consultative service. During these rotations, fellows quickly acquire the skills necessary to provide excellent patient care in a variety of clinical situations. Fellows work closely with a faculty member and provide direct care for patients in the CICU or in consultation.
In addition, fellows play a key role in the education of residents and medical students on service. As fellows progress through the program, they will assume more responsibility and require less direct faculty supervision. By the end of the inpatient rotations, fellows should be comfortable dealing with a variety of cardiac illnesses and will provide quality, evidence-based care.
Invasive cardiology
The invasive cardiology rotation offers an outstanding educational opportunity for fellows at the state-of-art catheterization laboratories at both Saint Luke’s Mid America Heart Institute and Truman Medical Center under the supervision of experts in diagnostic and interventional procedures. The fellows spend a minimum of four months in the catheterization laboratory with the option of spending more time if the fellow chooses to pursue further training in invasive cardiology. All diagnostic and interventional procedures are performed by board-certified interventional cardiologists, which allows fellows to learn techniques from highly experienced subspecialists in invasive/interventional cardiology.
Throughout the rotation, fellows are exposed to a high procedural volume allowing them to effectively learn the principles of invasive hemodynamic monitoring and left and right heart catheterization. Fellows perform diagnostic coronary angiographies and assist in a wide range of percutaneous coronary interventional procedures, peripheral vascular interventions, and structural heart interventions. As the fellows mature their skills, they will require less supervision by faculty members and will be able to perform diagnostic procedures independently.
The Mid America Heart Institute is a leading center in interventional cardiology, offering full service coronary angioplasty, including complex PCI procedures such as rotational atherectomy and chronic total occlusion intervention. The practice also maintains a high volume of vascular interventions, including endovascular aortic aneurysm repair, mesenteric, renal and lower extremity PTA, and venous interventions. Saint Luke's interventionalists perform more than 1,300 percutaneous interventions, 1,800 diagnostic catheterizations, and 440 peripheral interventions annually. The Heart Institute is also an active participant in several clinical trials of novel interventions. The program offers training in structural heart interventions, offering percutaneous atrial septal defect, PFO closure, left atrial appendage occlusion, and an active transcutaneous aortic valve replacement program. Fellows gain exposure to these techniques and will have an opportunity to pursue advanced training in interventional cardiology at the completion of their general cardiology training.
During catheterization rotations at Truman Medical Center, fellows have the unique opportunity to participate in a more hands-on fashion in interventional procedures. There are no interventional cardiology fellows at Truman Medical Center and interested general cardiology fellows are encouraged to begin learning interventional techniques from faculty. Fellows work closely with instructors on interventional procedures and have opportunities to participate in interventions in a variety of settings, including ST elevation myocardial infarction.

Echocardiography
Fellows have opportunities to learn fundamentals of echocardiography but also leading-edge echocardiographic methods, including 3D echocardiography, strain, and advanced structural echo. Four to five cardiologists daily serve as echo readers working in one of the busiest echo labs in the Midwest. All echo readers are certified by the National Board of Echocardiography.
Our faculty include members of the editorial board for the American Society of Echocardiography (ASE) and authors of ASE guidelines. Fellows benefit from novel blended learning methods (live teaching systematically enhanced with online learning) and weekly multidisciplinary case-based conferences. All fellows are required to spend a minimum of five months in the echo laboratory.
More dedicated time in echocardiography training is available for those who want more advanced learning.
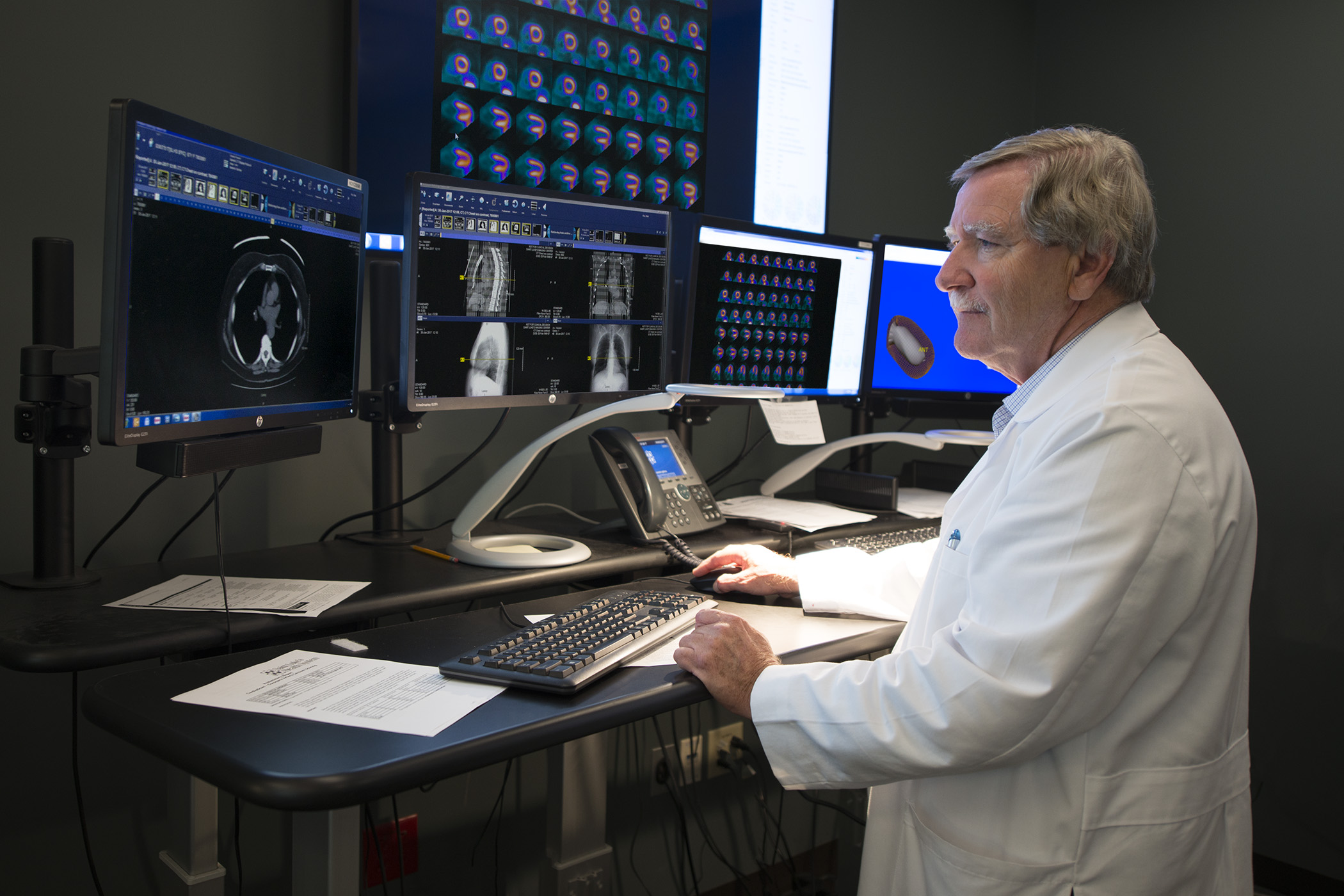
Advanced cardiovascular imaging
Fellows work directly with international leaders in advanced CV imaging, including former presidents, the current president-elect of the American Society of Nuclear Cardiology, and the current president of the Cardiovascular Council of the Society of Nuclear Medicine and Molecular Imaging. The Heart Institute pioneered one of the first cardiac positron emission tomography (PET) programs in the country almost 20 years ago, leading to ultra-high-quality images, and improved diagnostic accuracy and safety when compared with SPECT.
Fellows get first-hand experience in reading FDG PET’s (for cardiac sarcoid, myocarditis, and valve and device infections), cardiac amyloid scans, cardiac MRI, and cardiac and vascular CT. These studies are performed on cardiac-dedicated devices and all are interpreted by cardiologists, not radiologists.
Our faculty and fellows have authored or co-authored several hundred peer-reviewed publications and national guideline documents in advanced cardiac imaging, including work featured in The New York Times. A minimum of two months is required in the nuclear lab and at least one month of CT/MRI with the option of spending more dedicated time for those interested in obtaining higher levels of certification. We offer additional fellowship training in advanced cardiac imaging on a competitive basis.

Advanced heart failure and transplant
Saint Luke’s is one of the top 25 centers nationally for transplant volumes. More importantly, we are proud to be a national leader in heart-failure quality of care and patient outcomes as recognized by the American Heart Association Gold Plus designation. Our fellows directly benefit by learning to provide high-volume and high-quality advanced heart failure and transplant care. We also offer one position each year for an ACGME-accredited one-year advanced heart failure/transplant cardiology fellowship.
Clinical electrophysiology
Saint Luke’s electrophysiologists and fellows work together to annually perform more than 1,300 device implants, including leadless pacemakers, His-bundle pacemakers, and subcutaneous ICDs annually. Together, we also perform more than 700 catheter ablations, including many complex ablations for atypical flutter and epicardial ventricular tachycardia. Saint Luke’s was one of the first hospitals in the nation to utilize a novel 3D mapping system to non-invasively map the source of ventricular tachycardia and atrial fibrillation.
We also conduct ground-breaking clinic research through numerous clinical trials and registries. We host training courses for cryoablation as well as phrenic nerve pacemaker implantation for treatment of central sleep apnea. Fellows are required to spend two months on the clinical EP service. They may dedicate additional time to EP electives in the third year of training. We also offer two positions for an ACGME-accredited clinical cardiac electrophysiology fellowship.

Nuclear cardiology
As one of the busiest and most advanced nuclear stress laboratories in the country, cardiology fellows will gain extraordinary experience in the field of nuclear cardiology at the Heart Institute. During this rotation, fellows will be responsible for supervising and interpreting various nuclear stress tests, including SPECT and PET myocardial perfusion imaging, in addition to cardiac CT angiography, peripheral vascular CT angiography, and coronary artery calcium scanning, under direct supervision of cardiologists with specialized training in nuclear cardiology. Fellows are exposed to the latest techniques in nuclear imaging, including low dose protocols using state-of-the-art, solid-state CZT cameras and stress-only imaging protocols for appropriate patients.
Fellows gain further education during a weekly nuclear conference led by one of the nuclear cardiologists. A minimum of two months is required in the nuclear stress laboratory with the option of spending more dedicated time for those interested in obtaining a higher level of certification in nuclear cardiology.
Cardiovascular research
The Heart Institute boasts several active cardiovascular research programs, and publishes more than 100 articles in peer-reviewed journals annually. Each fellow is given at least three months of dedicated research time free from other clinical duties during their fellowship, with abundant opportunities to become more involved in research. Fellows are expected to complete at least one research project leading to either an abstract presentation at a national meeting or a peer-reviewed publication during their fellowship. The Cardiovascular Outcomes Research Group, led by John Spertus, MD, is one of the most productive cardiovascular outcomes research groups in the country.
The research groups at the Mid America Heart Institute all benefit from extensive support from research nurses, data collectors, and a large group of statisticians. Accordingly, rather than collecting data or abstracting charts, fellows can focus on developing questions, designing analyses collaboratively with faculty and statisticians, and writing papers.
The Health Outcomes and Technology Assessment group is active in economic analyses of new technologies and quality-of-life analyses concurrent with major clinical trials. Fellows may participate in weekly research meetings to discuss new or existing projects. There are also very active groups focusing on a host of areas, including interventional cardiology and cardiovascular imaging. The Heart Institute is an active participant in a variety of clinical trials, exposing fellows to leading therapies in the field. Interested fellows can pursue additional research training, including opportunities for advanced degrees in clinical research.
Select fellows with a strong interest in an academic career may also pursue a clinical investigator track pairing two years of cardiovascular outcomes research with the general cardiology fellowship.
Additional clinical elective experiences
- Adult Congenital Heart Disease Team: Host to a recurring regional conference in collaboration with Children’s Mercy Hospital
- Athletic Heart Clinic
- Autonomic Dysfunction Clinic
- ECMO Program
- Cardiac Amyloidosis Clinic
- Cardio-Oncology Team
- Cardio Metabolic Center of Excellence
- Cardiovascular and Thoracic Surgery
- Cardiovascular Anesthesia/CVICU
- Cardio Wellness (Preventive Cardiology) Clinic
- Heart Disease in Pregnancy Clinic: The first multidisciplinary clinic in the US for pregnant women with heart disease
- Valve Center of Excellence
- Vascular Center
- Women’s Heart Center
