Cerebrovascular Disorders
When you choose our care team, you have access to expert treatment for cerebrovascular diseases, which affect blood vessels in the brain. Thanks to our collaborative environment, you receive care from a multispecialty team of experts.
Stroke
What is a stroke?
A stroke, or brain attack, happens when blood flow to your brain is stopped. It's an emergency situation. Call
The brain needs a constant supply of oxygen and nutrients to work well. If the blood supply is stopped even for a short time, this can cause problems. Brain cells begin to die after just a few minutes without blood or oxygen.
When brain cells die, brain function is lost. You may not be able to do things that are controlled by that part of the brain. For example, a stroke may affect your ability to:
Move
Speak
Eat, drink, and swallow
See clearly
Think and remember
Solve problems
Control your bowel and bladder
Control your emotions
Control other vital body functions
A stroke can happen to anyone at any time.
What causes a stroke?
A stroke is caused when blood flow to your brain is stopped or disrupted.
There are 2 kinds of stroke, ischemic and hemorrhagic:
Ischemic stroke. This is the most common type of stroke. It happens when a blood vessel in the brain is blocked. It may be blocked by a blood clot. Or it may be blocked by a buildup of fatty deposit and cholesterol. This buildup is called plaque.
Hemorrhagic stroke. This occurs when a blood vessel in your brain bursts, spilling blood into nearby tissues. With a hemorrhagic stroke, pressure builds up in the nearby brain tissue. This causes even more damage and irritation.
Who is at risk for a stroke?
Anyone can have a stroke at any age. But your chance of having a stroke increases if you have certain risk factors. Some risk factors for stroke can be changed or managed, while others can’t.
Risk factors for stroke that can be changed, treated, or medically managed:
High blood pressure. Blood pressure of 140/90 mm/Hg or higher can damage blood vessels (arteries) that supply blood to the brain.
Heart disease. Heart disease is the second most important risk factor for stroke, and the major cause of death among survivors of stroke. Heart disease and stroke have many of the same risk factors.
Diabetes. People with diabetes are at greater risk for a stroke than someone without diabetes.
Smoking. Smoking almost doubles your risk for an ischemic stroke.
Birth control pills (oral contraceptives) Increases your risk for blood clots.
History of TIAs (transient ischemic attacks). TIAs are often called ministrokes. They have the same symptoms as stroke, but the symptoms don’t last. If you have had one or more TIAs, you are almost 10 times more likely to have a stroke than someone of the same age and sex who has not had a TIA.
High red blood cell count. A significant increase in the number of red blood cells thickens the blood and makes clots more likely. This raises the risk for stroke.
High blood cholesterol and lipids. High cholesterol levels can contribute to thickening or hardening of the arteries (atherosclerosis) caused by a buildup of plaque. Plaque is deposits of fatty substances, cholesterol, and calcium. Plaque buildup on the inside of the artery walls can decrease the amount of blood flow to the brain. A stroke occurs if the blood supply is cut off to the brain.
Lack of exercise
Obesity
Excessive alcohol use. More than 2 drinks per day raises your blood pressure. Binge drinking can lead to stroke.
Illegal drugs. IV (intravenous) drug abuse carries a high risk of stroke from blood clots (cerebral embolisms). Cocaine and other drugs have been closely linked to strokes, heart attacks, and many other cardiovascular problems.
Abnormal heart rhythm. Some types of heart disease can raise your risk for stroke. Having an irregular heartbeat (atrial fibrillation) is the most powerful and treatable heart risk factor of stroke.
Cardiac structural abnormalities. Damaged heart valves (valvular heart disease) can cause long-term (chronic) heart damage. Over time, this can raise your risk for stroke.
Risk factors for stroke that can’t be changed:
Older age. For each decade of life after age 55, your chance of having a stroke more than doubles.
Race. African Americans have a much higher risk for death and disability from a stroke than whites. This is partly because the African-American population has a greater incidence of high blood pressure.
Gender. Stroke occurs more often in men, but more women than men die from stroke.
History of prior stroke. You are at higher risk for having a second stroke after you have already had a stroke.
Heredity or genetics. The chance of stroke is greater in people with a family history of stroke.
Other risk factors include:
Where you live. Strokes are more common among people living in the southeastern U.S. than in other areas. This may be because of regional differences in lifestyle, race, smoking habits, and diet.
Temperature, season, and climate. Stroke deaths occur more often during extreme temperatures.
Social and economic factors. There is some evidence that strokes are more common among low-income people.
What are the symptoms of a stroke?
A stroke is an emergency situation. It’s important to know the signs of a stroke and get help quickly. Call
Stroke symptoms may happen suddenly. Each person’s symptoms may vary. Symptoms may include:
Weakness, drooping, or numbness of the face, arm, or leg, usually on one side of the body
Having trouble reading, speaking or understanding
Problems with vision, such as dimness or loss of vision in one or both eyes
Dizziness or problems with balance or coordination
Problems with movement or walking
Fainting (loss of consciousness) or seizure
Severe headaches with no known cause, especially if they happen suddenly
Other less common symptoms of stroke may include:
Sudden nausea or vomiting not caused by a viral illness
Brief loss or change of consciousness, such as fainting, confusion, seizures, or coma
TIA (ministroke)
A TIA is a serious condition and can cause many of the same symptoms as a stroke. But TIA symptoms pass, while stroke symptoms don't. They can last for a few minutes or up to 24 hours. Call for medical help right away if you think someone is having a TIA. An immediate medical evaluation is critical because the TIA symptoms may be a warning sign that a stroke is about to occur. But not all TIAs are followed by a stroke.
B.E. F.A.S.T for stroke
B.E. F.A.S.T. is an easy way to remember the signs of a stroke. When you see these signs, you will know that you need to call
B.E. F.A.S.T. stands for:
B - Balance. Sudden loss of balance or coordination.
E - Eyes. Vision changes in one or both eyes.
F - Face drooping. One side of the face is drooping or numb. When the person smiles, the smile is uneven.
A - Arm weakness. One arm is weak or numb. When the person lifts both arms at the same time, one arm may drift downward.
S - Speech difficulty. You may hear slurred speech or difficulty speaking. The person can't repeat a simple sentence correctly when asked.
T - Time to call 911. If someone shows any of these symptoms, call
How is a stroke diagnosed?
Your healthcare provider will take a complete health history and do a physical exam. You will need tests for stroke, such as brain imaging and measuring the blood flow in the brain. Tests may include:
CT scan of the brain. An imaging test that uses X-rays to take clear, detailed images of the brain. A brain CT scan can show bleeding in the brain or damage to brain cells caused by a stroke. It's used to find abnormalities and help find the location or type of stroke.
MRI. This test uses a combination of large magnets, radiofrequencies, and a computer to make detailed images of organs and structures in the body. An MRI uses magnetic fields to find small changes in brain tissue that help to find and diagnose stroke.
CTA (computed tomographic angiography). An X-ray image of the blood vessels. A CT angiogram uses CT technology to get images of blood vessels.
MRA (magnetic resonance angiography). This test uses MRI technology to check blood flow through the arteries.
Doppler sonography (carotid ultrasound). A test that uses sound waves to create pictures of the inside of your carotid arteries. This test can show if plaque has narrowed or blocked your carotid arteries.
Angiography. A catheter is inserted through your arteries. Dye is injected and pictures are taken.
The following heart tests may also be used to help diagnose heart problems that may have led to a stroke:
Electrocardiogram. This test records your heart’s electrical activity. It shows any irregular heart rhythms that may have caused a stroke.
Echocardiography. This test uses sound waves to create a picture of your heart. This test shows the size and shape of your heart. It can check if the heart valves are working correctly. It can also see if there are blood clots inside your heart.
How is a stroke treated?
Treatment will depend on your symptoms, age, and general health. It will also depend on how severe the condition is.
Advanced medical and surgical treatments are available. Some of these treatments can restore blood flow to the brain. Other treatments can help reduce your risk for another stroke.
Treatment is most effective when started right away. Emergency treatment after a stroke may include:
Clot-busting medicines (thrombolytics or fibrinolytics). These medicines dissolve the blood clots that cause an ischemic stroke. They can help reduce the damage to brain cells caused by the stroke. To be most effective, they must be given within 3 hours of a stroke occurring.
Medicines and therapy to reduce or control brain swelling. Special types of IV (intravenous) fluids are often used to help reduce or control brain swelling. They are used especially after a hemorrhagic stroke.
Neuroprotective medicines. These medicines help protect the brain from damage and lack of oxygen (ischemia).
Life support measures. These treatments include using a machine to help you breathe (a ventilator), having IV fluids, getting correct nutrition, and controlling your blood pressure.
Craniotomy. This is a type of brain surgery that is done to remove blood clots, relieve pressure, or repair bleeding in the brain.
What are possible complications of having a stroke?
Recovery from stroke and the specific ability affected depends on the size and location of the stroke.
A small stroke may cause problems, such as mild weakness in your arm or leg.
Larger strokes may cause parts of your body to not be able to move (be paralyzed). Larger strokes can also cause loss of speech or even death.
What can I do to prevent a stroke?
Know your risk for stroke. Many stroke risk factors can be changed, treated, or medically modified. Some things you can do to control your risk factors are listed below.
Lifestyle changes
A healthy lifestyle can help reduce your risk for stroke. That includes the following:
Stop smoking, if you smoke.
Make healthy food choices. Be sure to get the recommended amounts of fruits, vegetables, and whole grains. Choose foods that are low in animal fat, trans fat, cholesterol, salt (sodium), and added sugars.
Stay at a healthy weight.
Be physically active on a daily basis.
Limit alcohol use.
Medicines
Take your medicines as directed by your healthcare provider. The following medicines can help prevent stroke:
Blood-thinning medicines (anticoagulants) help prevent blood clots from forming. If you take a blood thinner, you may need regular blood tests.
Antiplatelets, such as aspirin, are prescribed for many stroke patients. They make blood clots less likely to form. Aspirin is available over the counter.
Blood-pressure medicines help lower high blood pressure. You may need to take more than one blood-pressure medicine.
Cholesterol-lowering drugs make plaque less likely to build up in your artery walls, which can reduce the risk for stroke.
Heart medicines can treat certain heart problems that increase your risk for stroke.
Diabetes medicines adjust blood sugar levels. This can prevent problems that lead to stroke.
Surgery
Several types of surgery may be done to help treat a stroke or help to prevent one. These include:
Carotid endarterectomy. Carotid endarterectomy is surgery to remove plaque and clots from the carotid arteries, located in the neck. These arteries supply the brain with blood from the heart. Endarterectomy may help stop a stroke from occurring.
Carotid stenting. A large metal coil (stent) is placed in the carotid artery much like a stent is placed in a coronary artery.
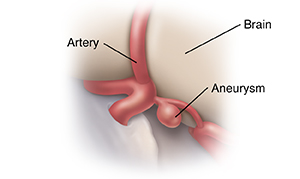
Surgery to repair aneurysms and AVMs (arteriovenous malformations). An aneurysm is a weakened, ballooned area on an artery wall. It's at risk for bursting (rupturing) and bleeding into the brain. An AVM is a tangle of arteries and veins. It interferes with blood circulation and puts you at risk for bleeding.
PFO (patent foramen ovale) closure. The foramen ovale is an opening that occurs in the wall between the 2 upper chambers of the heart. This opening usually closes right after birth. If the flap does not close, any clots or air bubbles can pass into the brain circulation. This can cause a stroke or TIA (transient ischemic attack). However, experts are still debating whether the PFO should be closed.
Heart surgery to close off part of the atrium (left atrial appendage closure) . This can reduce the risk for stroke from blood clots forming in the heart.
Living with a stroke
How a stroke affects you depends on where the stroke occurs in your brain. It also depends on how much your brain is damaged.
Many people who have a stroke are left with paralysis of one of their arms.
Other problems can include having trouble with:
Thinking
Speaking
Walking
Swallowing, eating, or drinking
Doing simple math, such as adding, subtracting, or balancing a checkbook
Basic problem solving
Dressing
Showering
Going to the bathroom
Some people may need long-term physical rehabilitation. They may not be able to live in their home without help.
Support services are available to help with physical and emotional needs after a stroke. This includes support services for caregivers.
When should I call my healthcare provider?
Strokes can happen again. Call
If you have repeated damage to your brain tissue, you may be at risk for life-long (permanent) disabilities.
Key points about stroke
A stroke happens when blood flow to your brain is stopped. It is an emergency situation.
It can be caused by a narrowed blood vessel, bleeding, or a clot that blocks blood flow.
Symptoms can happen suddenly. If someone is showing any sign of a stroke, call 911 immediately.
You have a better chance of recovering from a stroke if emergency treatment is started right away.
How a stroke affects you depends on where the stroke occurs in your brain, and on how much your brain is damaged.
A stroke can have serious impact on quality of life issues for both the person and their family. Support services are available for both the person and the caregiver.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
Know the reason for your visit and what you want to happen.
Before your visit, write down questions you want answered.
Bring someone with you to help you ask questions and remember what your provider tells you.
At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
Ask if your condition can be treated in other ways.
Know why a test or procedure is recommended and what the results could mean.
Know what to expect if you do not take the medicine or have the test or procedure.
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
Know how you can contact your provider if you have questions.
Arteriovenous Malformations
What are arteriovenous malformations?
Arteriovenous malformations (AVMs) are groups of blood vessels in your body that form in the wrong way. In AVMs, arteries and veins are abnormally tangled. This causes irregular connections between the arteries and veins.
AVMs can form anywhere in the body. But they most often occur in the spinal cord or brain. They often occur as the body develops before birth or shortly after. Those that form in the brain or close to the spinal cord are called neurological AVMs. These are most likely to have long-term effects. They may reduce the amount of oxygen getting to the brain and spinal cord. AVMs can also sometimes put pressure on nearby tissues.
Many people with an AVM don’t know they have one because they may not have any symptoms or problems. Instead, AVMs are often found when healthcare providers treat some other unrelated health concern. Or one of the blood vessels in an AVM may rupture, revealing the problem. Sometimes AVMs are found only after death, during an autopsy.
What causes arteriovenous malformations?
No one knows why AVMs form. Some experts believe that the risk of developing AVMs could be genetic.
What are the symptoms of arteriovenous malformations?
Many people with AVMs will never have any problems. If symptoms don't appear by age 50, they tend to remain stable. They are less likely to cause symptoms later in life.
Women may have symptoms as a result of pregnancy. Being pregnant may put pressure on the blood vessels.
Symptoms of an AVM depends on where it is located. You may have:
Buzzing or rushing sound in the ears
Headache—although no specific type of headache has been identified
Backache
Seizures
Loss of sensation in part of the body
Muscle weakness
Changes in vision
Facial paralysis
Drooping eyelids
Problems speaking
Changes in the sense of smell
Problems with motion
Dizziness
Loss of consciousness
How are arteriovenous malformations diagnosed?
Healthcare providers will ask about a person’s past health and symptoms. They will also do a physical exam. They may talk with family and friends about a person’s symptoms if they are unconscious.
The final diagnosis is often made based on imaging tests. These tests can show areas of blood flow:
Cerebral angiogram
MRI scan and magnetic resonance angiography
CT scan and CT angiography
Vascular ultrasound
How are arteriovenous malformations treated?
A treatment plan is developed based on the size and location of the AVM. Treatments may include:
Medicine for symptoms
Plugging off the malformed blood vessels (embolization)
Surgery (best when AVMs are small and located in superficial areas of the brain or spinal cord)
Radiation therapy (radiosurgery)
Talk with your healthcare provider about the risks and benefits of your treatment options.
What are possible complications of arteriovenous malformations?
The main concern with AVMs is that they may cause uncontrolled bleeding (hemorrhage). A small percentage of AVMs bleed. This can cause severe effects that may even result in death.
Other complications of AVMs are:
Stroke
Numbness in part of the body
Problems with speech or movement
Spinal fluid buildup in the brain (hydrocephalus)
Lower quality of life
Can arteriovenous malformations be prevented?
AVMs happen before birth or shortly after. Their cause is unknown. So you can’t prevent them. The best approach is to respond quickly to symptoms.
When should I call my healthcare provider?
Some people find out about an AVM only when it bleeds. This causes stroke in some people. Go right away to the emergency room or call 911 if you have these symptoms:
Seizure
Numbness
Vomiting
Physical weakness
Key points about arteriovenous malformations
Arteriovenous malformations (AVMs) are groups of blood vessels in your body that form in the wrong way.
AVMs often develop before birth or shortly after. The cause may be genetic.
Most people with AVMs will never have any problems.
If a person does have symptoms, it will depend on where the AVM is located. Symptoms may include headache, backache, seizures, or dizziness.
Imaging tests, such as an MRI or a CT scan, can often find an AVM.
Treatment options may include certain medicines or surgery.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
Know the reason for your visit and what you want to happen.
Before your visit, write down questions you want answered.
Bring someone with you to help you ask questions and remember what your provider tells you.
At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
Ask if your condition can be treated in other ways.
Know why a test or procedure is recommended and what the results could mean.
Know what to expect if you do not take the medicine or have the test or procedure.
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
Know how you can contact your healthcare provider if you have questions, especially after office hours or on weekends.
What Is a Brain Aneurysm?
An aneurysm is a bulge in the wall of an artery. Arteries are the blood vessels that carry blood to organs, such as the brain. A brain aneurysm can occur in an artery wall that is weak or has a defect. Brain aneurysms can occur at any age, but they are more common in adults than in children. They are also more common in women than in men.
Aneurysm is often linked with hardening of the arteries. Other risk factors include:
- High blood pressure.
- Family history.
- Smoking.
- Alcohol use.
- Cocaine use.
- Head injury.
- Certain health conditions, such as polycystic kidney disease.
If the bulge in a brain artery tears and bleeds, nearby brain tissue may be damaged. This can cause severe problems or death.
Symptoms
In most cases, a brain aneurysm has no symptoms until it bleeds or tears. Symptoms of rupture can include:
- A severe headache, usually of very sudden onset.
- Nausea and vomiting.
- A stiff neck.
- A brief blackout.
- Confusion.
- Slow movements.
- Clumsiness.
- Vision or speech problems.
- Paralysis or weakness on one side of the body.
- Jerking movements, such as seizures or convulsions.
- Coma.
Getting medical care fast
A health care provider needs to assess and treat a brain aneurysm right away, if possible. This may save the person's life. The care team will call specialists once they know the cause. Treatment will start right away if the aneurysm has bled.
In some cases, only supportive medical care may be used to treat bleeding. If the aneurysm has bled, treatment may not reverse damage to the brain. But surgery may help. It can prevent more bleeding. It can remove trapped blood in and around the brain. And it can relieve extra pressure on the brain. Or your provider may do other treatments. These include endovascular coiling or microvascular clipping. These can prevent more bleeding.
In some cases, an aneurysm can lead to severe brain injury. This may require medical life support. Sometimes even the most intensive treatment can’t save the person’s life.
Working with the health care team
Your loved one may be too ill to know what’s going on. You may need to decide on the extent of their treatment. The health care team will answer any questions you have. Choose only a few family members to talk to the care team. These family members can share what they learn with others. Doing this will make it simpler to keep everyone informed. If the situation is critical and your loved one has a living will or has designated someone with a medical power of attorney, be sure to let the care team know and provide copies of the documents.
Carotid Artery Disease
What is carotid artery disease?
The carotid arteries are the main blood vessels that send blood and oxygen to the brain. It's called carotid artery disease when these vessels become narrowed. It may also be called carotid artery stenosis.
Carotid artery disease reduces the flow of oxygen to the brain. The brain needs a constant supply of oxygen to work. Even a brief pause in blood supply can cause problems. Brain cells start to die after just a few minutes without blood or oxygen. A stroke can happen if the narrowing of the carotid arteries is bad enough that blood flow is blocked.
What causes carotid artery disease?
Atherosclerosis causes most carotid artery disease. Fatty deposits, calcium, fibrous tissue, and other cell debris build up along the lining of the arteries. This is called plaque. The plaque narrows the insides of the arteries. It reduces blood flow. Or it fully blocks the flow of blood to the brain. If a piece of plaque breaks off, it can also block blood flow to the brain. This too can cause a stroke.
Carotid artery disease is like coronary artery disease. In that disease, buildup occurs in the arteries of the heart. That may cause a heart attack.
Who is at risk for carotid artery disease?
Risk factors linked with atherosclerosis include:
Older age.
Biologically male.
Family history.
Race.
Genetic factors.
High cholesterol.
High blood pressure.
Smoking.
Diabetes.
Overweight.
Diet high in saturated fat.
Lack of exercise.
These factors increase a person's risk. But they don't always cause the disease. Knowing your risk factors can help you make lifestyle changes. You can work with your doctor to reduce the chance you will get the disease.
What are the symptoms of carotid artery disease?
The disease may have no symptoms. In some cases, the first sign of the disease is a transient ischemic attack (TIA) or stroke.
A TIA is a sudden, short-term loss of blood flow to a part of the brain. It usually lasts a few minutes to an hour. Symptoms go away fully within 24 hours. There are no lasting effects. When symptoms continue, it is a stroke. Symptoms of a TIA or stroke may include:
Sudden weakness or clumsiness of an arm or leg on one side of the body.
Sudden paralysis of an arm or leg on one side of the body.
Loss of coordination or movement.
Confusion, or loss of ability to concentrate.
Dizziness, fainting, or headache.
Numbness or loss of feeling in the face or in an arm or leg.
Temporary loss of vision or blurred vision.
Inability to speak clearly or slurred speech.
If you or a loved one has any of these symptoms, call for medical help right away. A TIA may be a warning sign that a stroke is about to occur. But TIAs don't always happen before strokes.
The symptoms of a TIA and stroke are the same. A stroke is loss of blood flow (ischemia) to the brain that lasts long enough to cause brain damage. Brain cells start to die after just a few minutes without oxygen.
The effects after a stroke depend on the size and place in the brain that had loss of blood flow. This may include problems with:
Moving.
Speaking.
Thinking.
Remembering.
Bowel and bladder function.
Eating.
Emotional control.
Other vital body functions.
Recovery also depends on the size and place of the stroke. A stroke may result in long-term problems, such as weakness in an arm or leg. It may cause paralysis, loss of speech, or even death.
The symptoms of carotid artery disease may look like other health problems. See your doctor for a diagnosis.
How is carotid artery disease diagnosed?
Your doctor will ask about your health history. They will do a physical exam. You will need tests. These may include:
Listening to the carotid arteries. For this test, your doctor places a stethoscope over the carotid artery. This is done to listen for a sound called a bruit (BREW-ee). This sound is made when blood passes through a narrowed artery. A bruit can be a sign of atherosclerosis. But an artery may be diseased and not make this sound.
Carotid artery duplex scan. This test is done to assess the blood flow of the carotid arteries. A probe called a transducer sends out ultrasonic sound waves. The transducer is also like a microphone. It is placed on the carotid arteries at certain locations and angles. The sound waves move through the skin and other body tissues to the blood vessels. The sound waves echo off the blood cells. The transducer sends the waves to an amplifier. Your doctor can hear the sound waves. Not enough or no sounds may mean blood flow is blocked.
MRI. This test makes detailed images of tissues in the body. It uses large magnets, radio waves, and a computer. X-rays are not used. For this test, you lie inside a big tube while magnets pass around your body. It’s very loud.
MR angiography. This test uses an MRI machine and I.V. contrast dye to make the blood vessels visible. The dye causes blood vessels to show up well on the MRI image. This is so the doctor can see them.
CT angiography (CTA). This test uses X-rays, a computer, and contrast dye. It makes detailed images of the body. A CTA shows pictures of blood vessels and tissues. It helps find narrowed blood vessels.
Angiography. This test is used to see how blocked the carotid arteries are. It is done by taking X-ray images while a contrast dye is injected. The contrast dye shows the shape and flow of blood through the arteries. X-ray images are made at the same time.
How is carotid artery disease treated?
Treatment will depend on your symptoms, age, and general health. It will also depend on how bad the condition is.
If a carotid artery is less than half narrowed, it is often treated with medicine and lifestyle changes. If the artery is between 50% and 70% narrowed, medicine or surgery may be done.
Treatment may include:
Lifestyle changes
Quit smoking. This can reduce the risk for carotid artery disease and heart disease. All nicotine products narrow the blood vessels. This includes electronic cigarettes. This decreases blood flow through the arteries.
Lower cholesterol. Eat a diet that is low in fat and cholesterol. Eat plenty of vegetables, lean meats (no red meats), fruits, and high-fiber grains. Don't eat processed foods. Also don't eat foods high in saturated fats and trans fats. If you can't control your cholesterol with diet and exercise, you may need medicines.
Lower blood sugar. High blood sugar (glucose) can cause damage to the lining of the carotid arteries. A diet that's low in sugar can help control blood sugar. So can regular exercise. If you have diabetes, you may need medicine or other treatment.
Exercise. Lack of exercise can cause weight gain. It can raise blood pressure and cholesterol. Exercise can help you keep a healthy weight. This can lower your risk for carotid artery disease.
Lower blood pressure. High blood pressure causes wear and tear and inflammation in blood vessels. This raises the risk for artery narrowing. Blood pressure should be below 140/90 mm/Hg for most people. People with diabetes may need even lower blood pressure.
Medicines
Medicines that may be used include:
Antiplatelets. These medicines make platelets in the blood less able to stick together and cause clots. They include aspirin, clopidogrel, and dipyridamole.
Cholesterol medicines. Statins are a type of medicine that lower cholesterol. They include simvastatin and atorvastatin. Studies have shown that some statins can decrease the thickness of the carotid artery wall. This can increase the size of the opening of the artery.
Blood pressure medicines. Several types of medicines work to lower blood pressure.
You may need stronger treatment if a carotid artery is narrowed from 50% to 70%. Especially if you have symptoms.
Surgery is usually advised for carotid narrowing of more than 70%. Surgery lowers the risk for stroke after symptoms. These include TIA or minor stroke.
Types of surgery include:
Carotid endarterectomy (CEA). This is surgery to remove plaque and blood clots from the carotid arteries. CEA may help prevent a stroke in people who have symptoms and a narrowing of 70% or more.
Carotid artery angioplasty with stenting. This is a choice for people who can't have CEA. It uses a very small tube (catheter). This tube is put into a blood vessel in the groin. It is pushed up to the carotid arteries. Once the tube is in place, a small balloon is inflated at the tip of it. This opens the artery. Then a stent is put in place. A stent is a thin, metal mesh tube. It is used to hold the artery open.
What are possible complications of carotid artery disease?
The main complication is a stroke. A stroke can cause serious problems. It may even cause death.
Can carotid artery disease be prevented?
You can prevent or delay the disease like you would prevent heart disease. This includes:
Diet changes. Eat a healthy diet. It should include plenty of fresh fruits and vegetables. Eat lean meats, such as poultry and fish. Eat low-fat or nonfat dairy foods. Limit your intake of salt, sugar, processed foods, saturated fats, and alcohol.
Exercise. Try for 30 minutes of moderate to vigorous physical activity 5 days per week, or as directed by your doctor. Start with 5 to 10 minutes at a time, if 30 minutes is too much for you. Any movement is better than none. Try to do exercises that strengthen your muscles 2 days per week. Examples of these are resistance bands or weights.
Managing your weight. If you are overweight, take steps to lose weight. Ask your doctor for help if you're not sure how to start.
Quitting smoking. If you smoke, quit. Enroll in a program to help you stop smoking. This can improve your chances of success. Ask your doctor about prescription medicine.
Controlling stress. Learn ways to manage stress in your home and work life.
When to contact your doctor
Learn the symptoms of a stroke. Have your family members also learn them. If you think you are having symptoms of a stroke, call 911 right away.
Key points about carotid artery disease
Carotid artery disease is when plaque builds up and causes narrowing of the carotid arteries. These arteries send oxygen-rich blood from the heart to the brain.
Narrowing of the carotid arteries can cause a stroke. Symptoms of a stroke should be treated right away.
Eating a healthy diet is one way to reduce the risk of the disease. Exercise, quitting smoking, blood pressure control, and medicine can also help.
Opening the carotid arteries can be done with surgery. Or it can be done with angioplasty and a stent.
A healthy lifestyle can help prevent or delay the disease.
The disease may not have symptoms. See your doctor for screening and diagnosis if you have important risk factors.
Next steps
Tips to help you get the most from a visit to your doctor:
Know the reason for your visit and what you want to happen.
Before your visit, write down questions you want answered.
Bring someone with you to help you ask questions and remember what your doctor tells you.
At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your doctor gives you.
Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
Ask if your condition can be treated in other ways.
Know why a test or procedure is recommended and what the results could mean.
Know what to expect if you do not take the medicine or have the test or procedure.
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
Know how you can contact your doctor if you have questions, especially after office hours or on weekends.
Subarachnoid Hemorrhage
What is a subarachnoid hemorrhage?
A subarachnoid hemorrhage is bleeding in the space between your brain and the membrane that covers it. Most often, it occurs when a weak area in a blood vessel (aneurysm) on the surface of the brain bursts and leaks. The blood then builds up around the brain and inside the skull. This increases pressure on the brain. It can cause brain cell damage, life-long problems, and disabilities.
When an aneurysm is located in the brain, it's called a cerebral, intracerebral, or intracranial aneurysm. A cerebral aneurysm often develops over a long period of time and may not cause any symptoms before it bursts (ruptures). Most aneurysms develop after age 40.
What causes a subarachnoid hemorrhage?
A subarachnoid hemorrhage may cause a type of stroke called a hemorrhagic stroke. This type of stroke causes bleeding inside the brain. Most subarachnoid hemorrhages are caused by bleeding after a brain aneurysm rupture. It is different from an ischemic stroke, which is caused by a blood clot.
This bleeding may go through the brain tissue and leak into the area outside the brain. This area is called the subarachnoid space. This can be life-threatening. The blood from the hemorrhage can compress or displace vital brain tissue. A severe hemorrhage can cause a coma. Or it can leave you paralyzed.
What are the symptoms of a subarachnoid hemorrhage?
Common symptoms include:
- Severe headache, the worst headache pain you've ever had that feels different from other headaches
- Loss of consciousness (may be brief or prolonged)
- Double vision
- Nausea or vomiting
- Trouble speaking
- Drooping eyelid
- Confusion and trouble concentrating
- Sensitivity to light
- Neck stiffness
- Neck pain
- Seizures
These symptoms may look like other health problems. Get medical care right away if you have these symptoms.
A brain aneurysm can lead to a subarachnoid hemorrhage. A brain aneurysm can cause these symptoms:
- Pain around the eye
- Changes in your vision, including double vision
- Dilated pupils
- Weakness or numbness on 1 side of your body
- Loss of hearing or trouble with balance
- Seizures
- Trouble with memory
How is a subarachnoid hemorrhage diagnosed?
If you have symptoms of a subarachnoid hemorrhage, you may need several tests for a diagnosis:
- CT scan. This test uses X-rays and a computer to make horizontal (axial) images of the brain. CT scans are more detailed than general X-rays.
- MRI scan. This test uses large magnets, radio waves, and a computer to make detailed images of the brain. It doesn't use X-rays.
- Angiogram. During this test, contrast dye is injected in the blood vessel. Then X-rays are taken to assess blood flow through them.
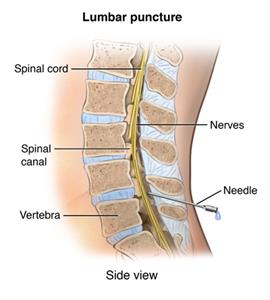
- Spinal tap. In this test, a special needle is placed into the low back, into the spinal canal. The pressure in the spinal canal and brain can be measured. A small amount of cerebrospinal fluid (CSF) can be removed. The CSF is checked for blood.
A diagnosis of a cerebral aneurysm isn't usually made until a subarachnoid hemorrhage has already occurred.
How is a subarachnoid hemorrhage treated?
A subarachnoid hemorrhage is a medical emergency. Immediate treatment is needed to help reduce the risk for lifelong brain damage. The main goal is to stop the bleeding and prevent rebleeding. Medicines may be started to prevent vasospasm and control high arterial pressure. Other medicines such as blood thinners (anticoagulants), will be stopped. Often, a healthcare provider may do surgery to place a small clip or stent on the blood vessel. This is to stop blood from leaking into the brain.
Some types of aneurysms can be treated with a detachable endovascular coil. This procedure is done by either a radiologist or a neurosurgeon. It is done with a tiny cut (incision) in your groin. A thin tube called a catheter is put through the incision into the artery in your leg. It is pushed up to the artery in your head that is bleeding. Recovery time from this type of treatment is much shorter than traditional surgery. But not all aneurysms can be treated this way. Your healthcare provider can determine if you are a candidate for this treatment after doing an angiogram.
Part of the long-term treatment of a subarachnoid hemorrhage includes addressing any risk factors that may have helped trigger the hemorrhage. One of the biggest risk factors is smoking. If you smoke, it's important to try to quit. Talk with your provider if you need help quitting. They can offer advice, support, and resources. Gaining better control of conditions such as diabetes, high cholesterol, or high blood pressure is also important. Keeping a healthy body weight and eating a healthy diet can also reduce your risk.
What are possible complications of a subarachnoid hemorrhage?
After a subarachnoid hemorrhage, serious complications can occur. Swelling in the brain (hydrocephalus) is one of the possible problems. It's caused by the buildup of CSF and blood between the brain and skull. This can increase the pressure on the brain. A subarachnoid hemorrhage can also irritate and damage the brain's other blood vessels, causing them to tighten. This reduces blood flow to the brain. As blood flow becomes affected, another stroke can happen. This can lead to even more brain damage. In serious cases, the bleeding may cause lifelong brain damage, paralysis, or coma.
When should I call my healthcare provider?
The sooner the bleeding in the brain is controlled, the better the outlook. Get emergency medical care if you have any signs such as:
- Seizures
- Severe headache; the worst headache pain that you have ever had
- Nausea and vomiting with the headache
- Double vision
- Neck stiffness
- Trouble speaking
- Drooping eyelid
- Confusion and trouble concentrating
- Sensitivity to light with the headache
Key points about a subarachnoid hemorrhage
- A subarachnoid hemorrhage means that there is bleeding in the space that surrounds the brain.
- It is life-threatening and a medical emergency.
- It often occurs in people older than age 40.
- One of the first symptoms is often having a severe headache. This is often followed by loss of consciousness.
- Get medical care right away if any of the above symptoms affect you or a loved one.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed and how it will help you. Also know what the side effects are and when you should report them to your healthcare provider.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.
What Is a Transient Ischemic Attack?
A transient ischemic attack (TIA), also called a ministroke or warning stroke, causes symptoms similar to those of a stroke. The difference is that TIAs don’t cause permanent brain damage, and they often last less than 5 minutes. But they can last up to 24 hours. About one-third of people will suffer a stroke in the year after a TIA.
TIAs happen when a blood clot or artery spasm suddenly blocks or closes off an artery briefly. This stops blood from reaching a part of the brain for a short period of time. Different parts of the brain do different things. So TIA symptoms depend on what part of the brain is affected. For example, a person can have weakness in their arm without the real problem being in the arm. The problem can be a lack of blood flow to the part of the brain that is responsible for arm strength.
Here are symptoms to watch for:
Sudden numbness in your face, arm, or leg, especially on 1 side of the body
Sudden confusion
Sudden trouble seeing, talking, or understanding
Sudden trouble with balance or walking
Sudden dizziness or loss of coordination
Sudden severe headache you can’t explain
Loss of consciousness or seizure
If you think you are having a TIA, get medical help right away. Recognizing symptoms of a TIA and getting treatment right away will reduce the risk for a major stroke.
Locations

Saint Luke's Neurology–Barry Road

Saint Luke's Neurology–Lee's Summit

Saint Luke's Neurology–Overland Park