Pediatric Diabetes Management and Endocrinology
Understanding Type 1 Diabetes
You’ve been told that your child has type 1 diabetes. This means their pancreas can't make insulin. In type 1 diabetes, an autoimmune disorder causes the body to destroy the cells in the pancreas that make insulin. Without enough insulin, blood sugar can't enter the cells to be used for energy. So, it builds up in the blood (hyperglycemia). Diabetes is a lifelong condition. Left untreated, it can lead to serious health problems. But diabetes can be managed with correct treatment and lifestyle changes. This lets your child live a full, healthy life.
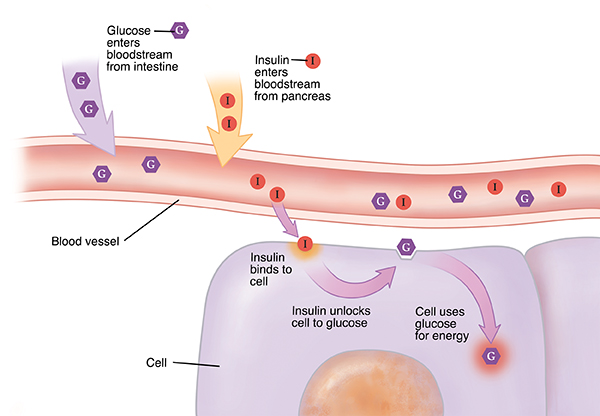
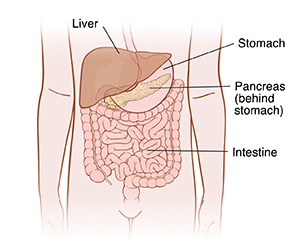
How the body gets energy
When your child eats, the digestive system breaks down food. Some of this food is turned into glucose in the intestine. Glucose (also called blood sugar) gives energy to the body’s cells. It travels through the blood to reach the cells. But glucose needs the help of a hormone called insulin to enter cells. Insulin is made by the pancreas. Insulin is released into the blood. It travels to the cells just like glucose. When insulin reaches a cell, it acts like a key. It opens a door into the cell so glucose can enter.
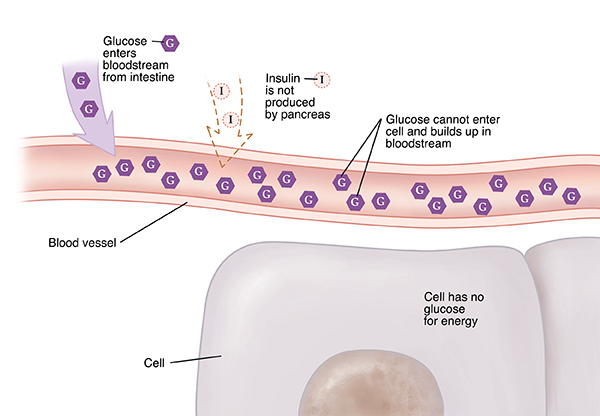
When your child has type 1 diabetes
In children with type 1 diabetes, the pancreas stops making insulin. Food is still broken down into glucose. And glucose still travels to the cells. But without insulin, glucose can’t enter the cells. Instead, it builds up in the blood. The liver puts more glucose out into the blood. Too much glucose in the blood is called hyperglycemia (high blood sugar). Without glucose, your child’s cells don’t get the energy they need. And over time, high blood sugar can cause other health problems.
What are the causes of type 1 diabetes?
The exact cause of type 1 diabetes isn't known. It occurs when the body's immune system starts targeting the insulin-producing cells in the pancreas. We do know that it’s not caused by eating too much sugar. Type 1 diabetes can run in families. Or your child may be the only person in the family to have type 1 diabetes. The important thing to remember is that it’s not your fault. Nothing you or your child did caused their diabetes. Having certain genes or being exposed to certain viruses may cause type 1 diabetes.
A new medicine was approved to help delay the onset of type 1 diabetes. This may be a choice for people ages 8 and older who are at high risk or have early signs of type 1 diabetes.
What are the symptoms of type 1 diabetes?
When the pancreas stops making insulin or makes very little insulin, the body’s cells become starved for energy. This can make your child feel tired and rundown. Your child may feel or have:
- Very strong thirst.
- Increased peeing.
- Blurry vision.
- Tired for no clear reason.
- Extreme hunger.
- Headaches.
- Flu-like symptoms.
- Bed wetting.
- Unexplained weight loss.
- Trouble focusing.
- Upset stomach (nausea), vomiting, and belly pain.
How is type 1 diabetes diagnosed?
Simple blood tests can help the doctor find out if your child has type 1 diabetes. These tests check for a high level of glucose in your child’s blood. Glucose tests may need to be repeated to confirm the diagnosis.
Your child's doctor may order other tests as well to confirm the diagnosis. These tests include levels of a substance called C-peptide and certain antibodies in the blood.
Autoantibody-based screening for type 1 diabetes before any symptoms show should be offered to those with a family history of type 1 diabetes.
How is type 1 diabetes treated?
There's no cure for type 1 diabetes. But it can be managed. Your child’s pancreas isn't making enough insulin. So insulin has to be put into your child’s body. Insulin is most often given as a shot. The idea of giving your child shots might seem scary at first. But most parents and children find that it’s easier than they thought. Insulin pens are accurate, easy to use and practically pain-free, even for children. Your child may be able to use an insulin pump that helps give insulin. Your child’s doctor will teach you how to check your child’s blood sugar level. This tells you how much insulin to give your child to keep blood sugar in a healthy range. Your child may be able to use a continuous glucose monitor to check their blood sugar level.
What are the long-term concerns?
People with a blood sugar level that's too high over many years can develop health problems. These problems can affect the heart, eyes, kidneys, and nerves. You can help delay or prevent these problems in your child. To do this, manage your child’s blood sugar as directed. Support and role model a healthy lifestyle. And teach your child in an age appropriate way how to manage their diabetes. Also, be aware of the symptoms of low blood sugar levels (hypoglycemia). These symptoms include headache, confusion, slurred speech, sweating, and irritable mood. Learn what to do when your child has low blood sugar. Teach other caregivers (such as those at your child's school or daycare) the same so that they may help in an emergency. Have your child wear a medical ID that says they have diabetes and whom to contact in case of an emergency.
The honeymoon phase
After diagnosis, your child’s pancreas may still be making a little insulin on its own. This is called the honeymoon phase. At this time, your child’s blood sugar may be managed with very little insulin. The honeymoon phase may last months or even years. Because of this, you may think that your child’s diabetes has gone away or been cured. But this isn't the case. As time goes on, your child’s pancreas will stop being able to make any insulin at all. Talk to your child’s doctor about managing your child’s blood sugar during the honeymoon phase.
Note
This sheet doesn't give all the information you need to care for your child with diabetes. Ask your child’s doctor for more information.
To learn more
For more information about diabetes, visit these websites:
- American Diabetes Association at www.diabetes.org
- Children with Diabetes at www.childrenwithdiabetes.org
- Juvenile Diabetes Research Foundation at www.jdrf.org
- American Association of Clinical Endocrinology at www.aace.com
- Endocrine Society at www.endocrine.org/topics/diabetes
- National Institute of Diabetes and Digestive and Kidney Diseases at www.niddk.nih.gov/health-information/diabetes
How daily issues affect your health
Many things in your daily life impact your health. This can include transportation, money problems, housing, access to food, and child care. If you can’t get to medical appointments, you may not receive the care you need. When money is tight, it may be difficult to pay for medicines. And living far from a grocery store can make it hard to buy healthy food.
If you have concerns in any of these or other areas, talk with your care team. They may know of local resources to assist you. Or they may have a staff person who can help.
Understanding Type 2 Diabetes
Your child has type 2 diabetes. This means their body has trouble using a sugar called glucose for energy. Diabetes is a lifelong condition. If not treated, it can lead to serious health problems. Diabetes can be managed so your child can live a full, healthy life. Type 2 diabetes has not been common in children, But, in recent years, more children are developing type 2 diabetes. This may be linked to a rise in childhood obesity.
How the body gets energy
When your child eats, their digestive system breaks down food. Some of this food is turned into glucose in the intestines. Glucose is also stored in and released by the liver. Glucose gives energy to the body’s cells. It travels through the blood to reach the cells. Glucose needs the help of a hormone called insulin to leave the blood and enter cells. Insulin is made by an organ called the pancreas. Insulin is released into the blood and travels to the cells just like glucose. When insulin reaches a cell, it acts like a key. It opens a “door” into the cell so glucose can enter.
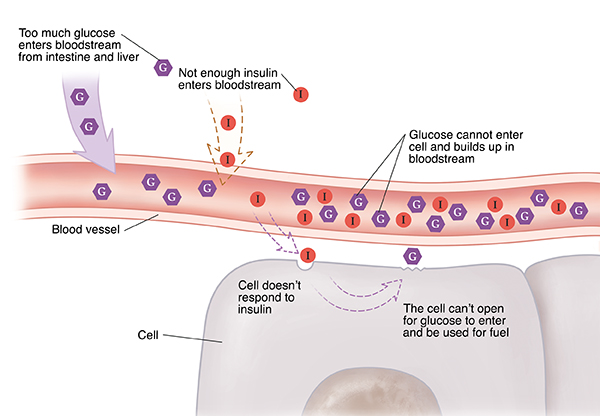
When your child has type 2 diabetes
With type 2 diabetes, food is still broken down into glucose. Glucose still travels to the cells. But the pancreas may not make enough insulin for the amount of glucose in the blood. The liver may release too much glucose at once. And the body’s cells may not respond the right way to insulin. This is called insulin resistance. Because of this, the cells get less glucose than they need. At first, the pancreas makes more insulin to try to keep up. As time passes, the pancreas can’t make enough insulin to overcome resistance. When this happens, glucose builds up in the bloodstream. Too much glucose in the blood is called hyperglycemia (high blood sugar). Without glucose getting into cells, your child’s cells don’t get the energy they need. Over time, high blood sugar can cause other more serious health problems.
What causes type 2 diabetes?
Type 2 diabetes often runs in families. African American, Latino, Native American, Asian American, and Pacific Islander families are often affected. Your child may be more likely to develop diabetes if:
They are female.
They spend more time sitting than being active.
They are overweight for age and height.
A parent or sibling has diabetes.
The mother had diabetes during pregnancy (gestational diabetes).
They had a low birth weight.
What are the symptoms of type 2 diabetes?
When your child has type 2 diabetes, the body’s cells become starved for energy. Most often, a child may not have any symptoms. Or your child may have symptoms, such as:
Being very thirsty.
Increased urination.
Blurry vision.
Tiredness during the day.
Extreme hunger.
Bed-wetting or getting up at night to urinate.
Weight gain or unexplained weight loss.
Trouble concentrating.
Vaginal infections caused by fungi.
Even if your child has no symptoms, high blood sugar can still be causing harm.
How is type 2 diabetes diagnosed?
Blood tests can help show if your child has type 2 diabetes. Your child may have tests, such as:
Hemoglobin A1C test. This test measures the average blood glucose for the past 2 to 3 months. An A1C of 6.5% or higher means your child has diabetes.
Fasting plasma glucose (FPG). This test checks blood glucose levels after 8 hours of fasting. Your child will have this test before their first meal of the day. This is called the fasting blood glucose level. A result higher than or equal to 126 mg/dl means your child has diabetes.
Oral glucose tolerance test (OGTT). For this test, your child's glucose level is measured before and then again 2 hours after having a sugary drink. This shows how well their body uses glucose. A result of 200 mg/dL or higher after 2 hours means your child has diabetes.
Random glucose test. This blood test is done at any time of the day. Blood glucose of 200 mg/dL or higher with symptoms of high blood sugar means your child has diabetes.
If your child doesn't have any symptoms of high blood sugar, they will need to have two abnormal test results from the same sample or in two separate test samples to be diagnosed. For example: Your child would need a fasting plasma glucose greater than 126 and an A1C greater than 6.5% from the same sample.
How is type 2 diabetes treated?
There is no cure for type 2 diabetes. But it can be managed. Your child’s doctor will work with you to create a treatment plan. Following the plan will help keep your child’s blood sugar in a healthy range. Type 2 diabetes is most often treated by:
Eating healthy meals.
Not having sugary drinks.
Being active.
Losing weight.
Taking medicine (if needed).
What are the long-term concerns?
People with a blood sugar level that is too high over many years can develop health problems. These problems can affect the heart, eyes, kidneys, and nerves. You CAN help delay or prevent these problems in your child. To do this, work with your care team to manage your child’s blood sugar as directed.
To learn more
For more information about diabetes, visit these websites:
American Diabetes Association www.diabetes.org
Children with Diabetes www.childrenwithdiabetes.org
Juvenile Diabetes Research Foundation www.jdrf.org
American Association of Diabetes Educators www.aadenet.org
American Association of Clinical Endocrinologists www.aace.com
National Diabetes Information Clearinghouse www.diabetes.niddk.nih.gov
How daily issues affect your health
Many things in your daily life impact your health. This can include transportation, money problems, housing, access to food, and child care. If you can’t get to medical appointments, you may not get the care you need. When money is tight, it may be hard to pay for medicines. And living far from a grocery store can make it hard to buy healthy food.
If you have any concerns, talk with your care team. They may know of local resources to help you. Or they may have a staff person who can help.
Follow up with your doctor
This sheet doesn't give all the information you need to care for your child with diabetes. Ask your child’s doctor for more information.
Locations