Kidney Cancer
Kidney cancer occurs when irregular cells grow in the kidneys, the two organs in the abdomen that filter waste from your blood. Our specialists use advanced techniques to treat cancer and restore kidney function, preserving the kidney whenever possible.
What is cancer?
Cancer is when cells in the body change and grow out of control. To help you understand what happens when you have cancer, let’s look at how your body works normally. Your body is made up of tiny building blocks called cells. Normal cells grow when your body needs them. They die when your body does not need them any longer.
Cancer is made up of abnormal cells that grow even though your body doesn’t need them. In most cancers, the abnormal cells grow to form a lump or mass called a tumor. If cancer cells are in the body long enough, they can grow into (invade) nearby areas. They can even spread to other parts of the body (metastasis).
What is kidney cancer?
Cancer that starts in kidney cells is called kidney or renal cancer.
Understanding the kidneys
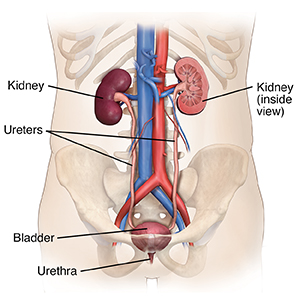
The kidneys are 2 bean-shaped organs. Each is about the size of a bar of soap. They sit just below the rib cage, toward the middle of the back. There is 1 kidney on each side of the spine. The kidneys help filter waste and excess fluid from the blood. The liquid and waste are then sent as urine to the bladder through thin tubes (ureters). Urine then leaves the body through a tube called the urethra. The kidneys also help control blood pressure. And they help make sure there are enough red blood cells in the body.
When kidney cancer forms
A kidney is made up of many layers of cells. Kidney cancer can affect any one or all of these layers. The cancer can stop the kidneys from working normally. Kidney cancer may spread to other parts of the body. When cancer spreads, it’s called metastasis. The more cancer spreads (metastasizes), the harder it is to treat.
What are the different types of kidney cancer?
The main type of kidney cancer is called renal cell carcinoma (RCC). About 9 out of 10 kidney cancer tumors are this type. If you have this type of kidney cancer, you will usually have only 1 tumor in 1 kidney. But there may be more than 1 tumor in 1 kidney or in both kidneys. These may be large by the time they are diagnosed. But most cases of kidney cancer are found before the cancer has spread to other organs.
There are many different types of RCC. A healthcare provider called a pathologist identifies these types by looking at the cancer cells under a microscope. The types of RCC include:
- Clear cell. This is the most common subtype of RCC. The cancer cells look pale or clear.
- Papillary. This is the second most common type of RCC and most common type of non-clear cell RCC. This type of tumor has tiny, fingerlike growths.
- Chromophobe. This is a rare form of RCC. The cells are pale and larger than other types of RCC.
- Collecting duct. This is also a rare form of RCC. The cancer forms in cells of the collecting ducts or tubules.
- Medullary. This is a rare and aggressive type of RCC that mostly occurs in young people of African descent with sickle-cell trait or disease.
- Unclassified. This includes tumors that have cells from more than 1 type of cancer. It also includes tumors with cells that don’t fit into the other categories.
Other types of kidney cancer
Other less common types of kidney cancers include:
- Transitional cell carcinoma. This is also known as urothelial carcinoma. It starts where the ureter and kidney meet. This area is called the renal pelvis. This type of kidney cancer can act and look like bladder cancer.
- Wilms tumor. Also called nephroblastoma, this cancer most always occurs in children. It's very rare in adults.
- Renal sarcoma. This is a very rare type of kidney cancer. It begins in the blood vessels and connective tissue around the kidneys.
Kidney tumors that aren’t cancer
There are several types of kidney tumors that are not cancer (benign). These include renal cell adenoma, renal oncocytoma, and angiomyolipoma. These types of tumors may still affect kidney function and can cause pain and other symptoms. But the cells often do not spread to other organs.
Talk with your healthcare provider
If you have questions about kidney cancer, talk with your healthcare provider. Your healthcare provider can help you understand more about this cancer.
What are the symptoms of kidney cancer?
Kidney cancer often causes no symptoms in its early stages (when it's small and hasn't spread). As the cancer grows, it can cause symptoms, such as:
- Blood in the urine. Blood in the urine (hematuria) is one of the most common signs of kidney cancer. You may be able to see the blood easily in your urine. Or the blood cells may show up only when a urine test is done.
- Pain in the side or lower back. Side and back pains can be caused by the tumor growing and pushing against nearby organs. It may feel like pressure also. It's usually felt on one side only.
- A lump in the kidney area. If you feel a lump in the kidney area (your lower back or side) and have not had an injury, a cancer mass may be there. The lump may hurt.
- Tiredness. Tiredness that doesn't get better with rest is a common problem for people with cancer. It's often caused by a low number of red blood cells (anemia).
- Fast weight loss. Weight loss that happens quickly without any effort can be a sign of kidney cancer.
- Loss of appetite
- Swelling of the legs and ankles
- Fever not caused by an infection or that comes back
- High blood pressure
- A cluster of swollen blood vessels around a testicle that develops quickly
- Bone pain, difficulty breathing, and headache. These are symptoms caused by the distant spread to other organs or tissue.
When to see your healthcare provider
Many of these symptoms may be caused by other health problems. Still, it's important to see a healthcare provider if you have these symptoms. Only a healthcare provider can tell if you have cancer.
How is kidney cancer diagnosed?
Diagnosing kidney cancer starts with your healthcare provider asking you questions. They will ask about your health history, your symptoms, risk factors, and family history of disease.
Your healthcare provider will also give you a physical exam. You may be checked for a fever and high blood pressure. The healthcare provider may feel your belly (abdomen), sides, and back for lumps.
What tests might I need?
Symptoms of kidney cancer can be caused by other less serious problems. Because of this, you will likely have some tests. Unlike most types of cancer, kidney cancer can often be diagnosed without a biopsy. A biopsy is when small pieces of tissue are removed and looked at with a microscope. Instead, you may have one or more of the following:
- Urine test
- Blood tests
- CT scan
- MRI scan
- Ultrasound
- Intravenous pyelogram (IVP)
- Angiography
- Fine needle aspiration or biopsy
Urine test
About 2 out of 5 people with kidney cancer, where the cancer has invaded the kidneys' collecting system, have blood in their urine. But there are many conditions that may cause blood in the urine. Check with your healthcare provider. Blood in the urine can be found by doing a test called a urinalysis. For this test, a small sample of your urine is tested in a lab to see if it has blood. Your healthcare provider may do a special kind of urine test (urine cytology). It checks for cancer cells in the urine.
Blood tests
There is no blood test that can diagnose kidney cancer. But a complete blood count (CBC), blood comprehensive metabolic panel (CMP), and other chemistry tests can show signs in the blood that are linked with kidney cancer. They will also check how well your organs are working. For example:
- Too few red blood cells. This condition is called anemia. It is common in many kinds of cancer.
- Too many red blood cells. This condition is called erythrocytosis or polycythemia. Some types of kidney cancer cells make a hormone called erythropoietin. This causes bone marrow to make too many blood cells.
- A high blood calcium level. This may show that the cancer has begun to affect the bones.
- Lactate dehydrogenase (LDH). This enzyme may be increased when fast-growing cells like cancer cells die.
- A high level of liver enzymes. This may be a sign that the cancer has spread to the liver.
Imaging Tests
CT scan
A CT scan uses a series of X-rays from different angles and a computer to make detailed images of the inside of the body. This test can confirm a diagnosis of kidney cancer. During the test, you lie still on a table as it slides into a CT scanner. A CT scan is painless. You may be asked to hold your breath one or more times during the scan.
In some cases, you will be asked to drink a contrast material (sometimes called dye) 4 to 6 hours before the scan. Then you may be asked not to eat anything until a second set of pictures is taken. The contrast lets your healthcare provider see certain parts of the body more clearly. The contrast will pass through your body and exit through your urine and bowel movements. Contrast may be given by injection into a vein as well. When the contrast is injected, you may have a warm feeling from your chest to your groin. Tell your healthcare provider if you have ever had a reaction to contrast materials. This includes hives, trouble breathing, or becoming suddenly hot. Special medicines can be given before the test to help prevent these kinds of reactions.
MRI scan
An MRI uses radio waves, large, strong magnets, and a computer to create detailed images of the body. It does not use X-rays. An MRI can show if the cancer has grown into major blood vessels (such as the renal vein and inferior vena cava) or spread to your spine or brain.
You may receive contrast through a vein before the MRI scan. During the test, you lie still on a table as it passes into a scanner tube. If you can’t handle small, enclosed spaces (feeling claustrophobic), you may be given a sedative before having this test. The scanner takes 2 to 15 minutes to make an image. You may need more than one set of images. The test may last an hour or more. An MRI test is painless. But it is noisy. You can bring earphones and a music device, or ask for earplugs.
Ultrasound
An ultrasound test uses high-energy sound waves to create images on a computer screen. An ultrasound does not use X-rays and is painless. A gel is put on the skin of your lower back or abdomen. A technician then uses a handheld wand (called a probe or transducer) to press on the skin above your kidneys. This test can help show if a kidney tumor is a fluid-filled sac (cyst) or a solid tumor. It can also show if the tumor has blood flowing through it. A solid tumor with blood flow is more likely to be cancer.
Intravenous pyelogram (IVP)
This test uses a special contrast material (also called agent) and X-rays to look at the kidneys, ureters, and bladder. During this test, your healthcare provider injects contrast into one of your veins. X-rays are taken as the contrast passes through your urinary tract. With the help of the contrast, your healthcare provider can see abnormal things, tumors, kidney stones, or any blocked areas that may be caused by kidney cancer. The test can also check the blood flow through the kidneys.
Angiography
This test is very much like an IVP. It uses contrast material and X-rays to look at the kidneys. This test is usually done as part of a CT scan or MRI scan to use less contrast (excess contrast can damage kidney function). With angiography, the contrast is injected directly into a renal artery that goes to your kidney. The test helps show the blood vessels and lets your healthcare provider see which blood vessels are sending blood to the tumor. This test can also help your healthcare provider see if the tumor can be taken out by surgery.
Biopsy
Fine needle aspiration (FNA) or core needle biopsy
A biopsy is a test to take small pieces of tissue from the body. The tissue is then looked at with a microscope. A biopsy is not often done for kidney cancer. In most cases, imaging tests and surgery give all the information needed to diagnose and treat the cancer. But in some cases, a biopsy may be done to confirm a diagnosis of kidney cancer. It can also give more information to help your healthcare provider decide which treatment is best.
During a biopsy, your skin is numbed. A thin needle is then inserted through your skin to remove fluid or small pieces of tissue from your kidney. Ultrasound may be used to guide the needle biopsy. Your healthcare provider then sends the sample to a specialist, called a pathologist. The pathologist then looks for abnormal cells under a microscope. It often takes several days for the results of a biopsy to come back. The healthcare provider may request biomarker lab tests on the tissue to check for specific proteins, genes, mutations, and other features unique to kidney cancers. The results may help with treatment choices.
The difference between an FNA and a biopsy can be subtle. An FNA involves sucking (aspirating) a small amount of tissue or fluid through a needle using a syringe. The needle used for FNA biopsy is thinner than the ones used for routine blood tests. The needle used in core biopsies is larger than that used in an FNA. It removes a small cylinder of tissue.
Surgery
Surgery is the most common treatment for kidney cancer. The goal is to take out the tumor or tumors. Sometimes the entire kidney is removed. Nearby lymph nodes might be taken out, too.
When might surgery be used to treat kidney cancer?
Your healthcare provider may advise surgery to treat your kidney cancer if:
- You are healthy enough to have surgery. Your healthcare provider will only advise surgery if they expect you to be able to recover from it.
- The tumor is small. In this case, a partial nephrectomy might be done. This allows you to keep some kidney function. Only the part of the kidney that contains the tumor and some kidney tissue surrounding the tumor is taken out. This surgery is done if you have only one small tumor in one kidney. It may also be done if the tumor is larger, but you have cancer in both kidneys or you only have one kidney. The benefit is that you keep part of your kidney. The risk is that there's a chance some cancer cells will be left behind.
- The tumor is large but is only in your kidney. The type of surgery you need is based on how big the tumor is and where it is.
- One choice is a simple nephrectomy. This is surgery to take out the entire kidney.
- Or your healthcare provider may advise a radical nephrectomy. This is where the whole kidney, the adrenal gland (attached to the top of the kidney with the cancer), and nearby fatty tissues are removed. The surgeon might not remove the adrenal gland if it looks normal on imaging tests or the cancer is not high risk. . Nearby lymph nodes may also be removed in a procedure called lymph node dissection. They are removed when the provider can feel or see the enlarged lymph nodes on imaging tests done before surgery. This is done because cancer tends to travel to the nodes first. Taking them out may help keep cancer from spreading to other parts of your body. And testing these lymph nodes helps figure out the stage of the cancer. This is important in deciding if other treatments are needed after surgery.
- You have kidney cancer that has spread to only one other area. Your healthcare provider may suggest a radical nephrectomy and removal of the tumors in other parts of your body. This may not cure the cancer. But it can help ease symptoms, like pressure, pain, or bleeding.
- You have symptoms. You may have pain, pressure, or bleeding from tumors that have spread. Your healthcare provider might suggest surgery to remove those tumors. This is done to ease symptoms. It doesn't cure the cancer. You may hear it called palliative surgery.
Types of surgery
Kidney cancer surgery may be done in many ways. The type of surgery done depends on how big the tumor is and where it is in the kidney:
- Open surgery. This is done through a large cut (incision) made in the skin, fat, and muscle over the belly (abdomen). Or the incision might be made on your side, below your ribs, or your back. One of your lower ribs may need to be taken out to reach the kidney. The surgery is then done through this incision.
Minimally invasive surgery:
- Laparoscopy. This type of surgery is done through many small incisions in your skin. A thin, flexible tube with a light and camera on the end (called a laparoscope) is put into one incision. Long, thin tools are then put into the other incisions to do the surgery. Laparoscopy often leads to less time in the hospital after surgery. It tends to cause less pain and scarring and has a faster recovery.
- Robotic-assisted surgery. This type of surgery is like laparoscopic surgery, but it's done by robot arms that are guided by a surgeon who sits at a computer panel. It's only done at certain surgery centers. And it should be done only by a healthcare provider with training and a lot of experience. This type of surgery uses smaller incisions and may lead to less pain and scarring after surgery.
Risks of kidney cancer surgery
All surgery has risks. The risks of kidney surgery include:
- Excess bleeding
- Infection
- Damage to nearby internal organs and blood vessels
- Bulging of organs under the incision (hernia)
- Air in the chest cavity (pneumothorax)
- Kidney failure of the remaining kidney
- Urine leaking into the abdomen after partial nephrectomy
Your risks depend on your overall health, the type of surgery you need, and other factors. Talk with your healthcare provider about which risks apply most to you.
Getting ready for your surgery
Your healthcare team will talk with you about the surgery choices that are best for you. You may want to bring a family member or close friend with you to appointments. Write down questions you want to ask about your surgery. Make sure to ask:
- What type of surgery will be done
- What will be done during surgery
- The risks and possible side effects of the surgery
- If you'll have kidney function after surgery (or if you will need dialysis)
- When you can go back to doing your normal activities
- If the surgery will leave scars and what they'll look like
Before surgery, tell your healthcare team if you are taking any medicines. This includes prescription and over-the-counter medicines, vitamins, herbs, and other supplements. It also includes marijuana or illegal drugs. This is to make sure you’re not taking anything that could affect the surgery. After you've discussed all the details with the surgeon, you'll sign a consent form that says that the healthcare provider can do the surgery.
You’ll also meet the anesthesiologist and can ask questions about the anesthesia and how it will affect you. Be sure to tell your healthcare provider if you had problems with anesthesia in the past. Before surgery starts, an anesthesiologist or a nurse anesthetist will give you certain medicines (called anesthesia) that make you fall asleep so you don’t feel pain.
After your surgery
You'll wake up in a recovery room. You'll be watched closely as you fully wake up and are able to talk to the nurses. You may have to stay in the hospital for about 1 to 7 days, depending on the type of surgery you had.
For the first few days after surgery, you're likely to have pain from the incision. Your pain can be controlled with medicine. Talk with your healthcare provider or nurse about your choices for pain relief. Some people don’t want to take pain medicine, but doing so can help you recover and heal. For instance, if you don’t control pain well, you may not want to cough, turn often, or get out of bed, all of which you need to do as you recover from surgery.
It may be uncomfortable to breathe deeply after surgery. You will be asked to do deep breathing exercises to keep you from getting a lung infection (pneumonia),
You will likely have a urinary catheter for a few days. This is a tube put through your urethra (the tube that carries urine out of your body) and into your bladder so that your urine drains into a bag outside your body. You may go home with the catheter for a while.
You may have bowel problems right after surgery. If you have diarrhea, ask what you can do about it. Sometimes diet changes can help. Constipation is common from using certain pain medicines, not moving much, or not eating and drinking as much as usual. Talk with your healthcare provider or nurse about getting more dietary fiber or using a stool softener.
Recovering at home
When you get home, you may get back to light activity within a week or two. You should not do any strenuous activity or heavy lifting for at least 6 weeks.
You may feel sore, tired or weak for a while. The amount of time it takes to recover from surgery is different for each person. But you may not feel like yourself for a few months. You'll be able to get your incision wet in the shower. But to reduce your risk of infection, don’t take baths or swim. Ask your healthcare provider when it's OK for you to drive.
Your healthcare team will tell you what kinds of activities are safe for you while you recover.
Follow-up care
Your healthcare provider will use blood tests to follow how well your remaining kidney works. You may need more treatment after surgery. This will not start until you've had time to heal. Your healthcare provider will talk with you about the next steps of treatment and when it will start. Make sure you know what to do and make a follow-up appointment.
When to call your healthcare provider
You may need to take medicine when you go home, such as pain medicine or antibiotics. It's important to know what you're taking. Get a written list of the names of all your medicines. Ask your healthcare team how to take them, how they work, what they're for, and what side effects they might cause.
Talk with your healthcare providers about what problems to watch for and when to call them. Call right away if you have any of these problems after surgery:
- Bleeding
- New pain or pain that's worse
- Redness, swelling, warmth, or fluid leaking from the incision
- Incision opens up or the edges pull apart
- Fever of 100.4°F (38°C) or higher, or as advised by your healthcare provider
- Chills
- Changes in how much urine you're making or changes in how it looks or smells
- Cough or shortness of breath
- Rapid, irregular heartbeat; new chest pain
- Pain, redness, swelling, or warmth in an arm or leg
Make sure you know who and what number to call with problems or questions. Also be sure you know what number to call to get help after office hours and on weekends and holidays.