Rectal Bleeding
Understanding Rectal Bleeding
Understanding Rectal Bleeding
Rectal bleeding is when blood passes through your rectum and anus. It can happen with or without a bowel movement. Rectal bleeding may be a sign of a serious problem in your rectum, colon, or upper GI tract. Call your healthcare provider right away if you have any rectal bleeding.
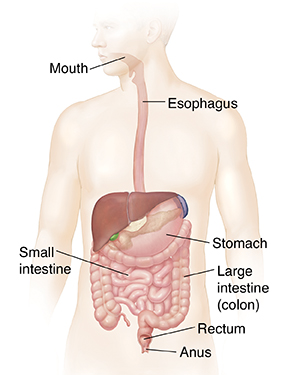
The GI tract
The gastrointestinal (GI) tract includes the:
- Mouth
- Esophagus
- Stomach
- Small intestine
- Large intestine (colon)
- Rectum
- Anus
The food you eat is digested as it passes through the GI tract. Solid waste leaves the body through the rectum and anus.
Rectal bleeding and GI problems
The cause of rectal bleeding may be found in any part of the GI tract. The colon or rectum may be the site of your bleeding problem. Or bleeding may be due to problems farther up the GI tract, such as in the small intestine, duodenum, or stomach.
Causes of rectal bleeding
These are some possible causes:
-
Swollen veins in the rectum and anus (hemorrhoids)
-
Tears in or near the anus (fissures)
-
Pockets in the colon wall that can bleed (diverticulosis)
-
Infection
-
Low blood flow (ischemia)
-
Radiation damage
-
Inflammatory bowel disease (Crohn's disease or ulcerative colitis)
-
Ulcers in the upper GI tract and inflammation of the large intestine
-
Abnormal tissue growths (cancer tumors or polyps) in the GI tract
-
A bulging rectum (rectal prolapse)
-
Abnormal blood vessels in the small intestine or in the colon
Common symptoms
Common symptoms are:
-
Rectal pain, itching, or soreness
-
Belly pain, including upper belly pain near the stomach (epigastric pain)
-
Small drops of blood that sometimes are seen on the stool or toilet paper
-
Stool that looks black or tarry
Rectal bleeding can also happen without pain.
Evaluating and Treating Rectal Bleeding
Evaluating and Treating Rectal Bleeding
To find the site and cause of your bleeding, you'll have a physical exam. You'll be asked about your health history. Tests may be done to help confirm the diagnosis and plan your treatment.
Tests you may have
You will have blood work done. You may also have these tests:
-
Stool sample. A small amount of your stool will be checked for blood.
-
Anoscopy. This test uses a small tube (anoscope) to examine the anus. It checks for problems, such as hemorrhoids.
-
Sigmoidoscopy. This test uses a lighted tube to check your rectum and the part of the large intestine that's closest to the rectum (the sigmoid colon).
-
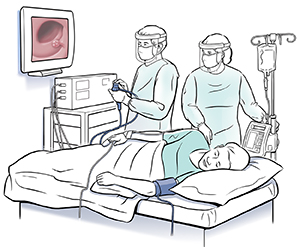
Colonoscopy. This test looks at your rectum and entire colon. You will be given medicine through an IV (intravenous) line to help you relax.
-
Lower GI (gastrointestinal) series, or barium enema. This is an X-ray test to view your colon. A milky liquid containing barium is passed through your rectum and into the colon. This liquid makes it easy to see your colon on the X-ray. This test is not done that often anymore.
-
Upper endoscopy. This test checks your esophagus, stomach, and upper small intestine. It's done in cases of rectal bleeding along with other symptoms like low blood pressure and rapid heartbeat. This test may also be done if your stools are dark black and tarry.
-
Capsule endoscopy. For this test, you swallow a pill that has a tiny camera inside. The camera takes pictures of your small intestine. It can get to areas that are hard to reach with colonoscopy and upper endoscopy.
-
Balloon or spiral enteroscopy. These tests use a special tube (scope) to get deep into the small intestine.
-
Tagged red blood cell scan. This test marks (tags) red blood cells with very small amounts of radioactive material. The cells can then be seen and tracked on a scan.
-
Angiography. This test threads a tube (catheter) through a vein, often in the leg. Dye is injected through the tube into your blood vessels to see where the bleeding is taking place.
Your treatment plan
Your treatment will depend on the cause of your rectal bleeding, as well as the severity of the bleeding. Your healthcare provider will create a treatment plan that’s right for you. Sometimes rectal bleeding stops on its own. Either way, be sure to see your provider to find the cause of the problem.
What you can do
Follow all your healthcare provider’s instructions. Keep working with your provider after your treatment. Make and keep your follow-up visits. If you have more rectal bleeding, call your provider. It may be a sign of the same or another health problem.
Understanding Colon and Rectal Polyps
Understanding Colon and Rectal Polyps
The colon (also called the large intestine) is a muscular tube that forms the last part of the digestive tract. It absorbs water and stores food waste. The colon is about 4 to 6 feet long. The rectum is the last 6 inches of the colon. The colon and rectum have a smooth lining composed of millions of cells. Changes in these cells can lead to growths called polyps in the colon. These can become cancerous and should be removed. Many tests are available to screen for colon cancer. But colonoscopy is the only test that looks directly into the entire large intestine and allows for treatment right away. During colonoscopy, these polyps can be removed. How often you need this test depends on many things. These include your condition, your family history, symptoms, and what the findings were at the previous colonoscopy.
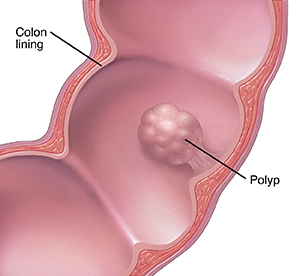
When the colon lining changes
Changes that happen in the cells that line the colon or rectum can lead to growths called polyps. Over a period of years, polyps can turn into cancer. Removing polyps early may prevent cancer from ever forming.
Polyps
Polyps are fleshy clumps of tissue that form on the lining of the colon or rectum. Small polyps are usually not cancer (benign). But over time, cells in a polyp can change and become precancerous. Certain types of polyps known as adenomatous polyps and serrated polyps are precancerous. The risk for cancer also increases with the size of the polyp and certain cell and gene features. This means that they may become cancerous if they're not removed. Hyperplastic polyps are benign. They can grow quite large and not turn cancerous.
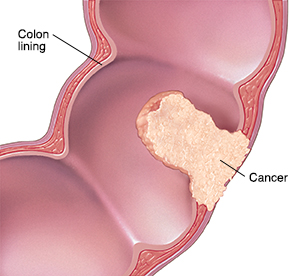
Cancer
Almost all colorectal cancers start when polyp cells start growing abnormally. As a cancerous tumor grows, it may affect more and more of the colon or rectum. In time, cancer can also grow beyond the colon or rectum and spread to nearby organs or to glands called lymph nodes. The cells can also travel to other parts of the body. This is known as metastasis. The earlier a cancerous tumor is removed, the better the chance of preventing its spread.
Providers
Benjamin J Kulow, MD
