Breast Cancer
Breast cancer has a nearly 100 percent survival rate when caught early. The key is accurate detection, expert diagnosis, personalized treatment options, and survivorship support for every patient. It’s what Saint Luke’s calls precision medicine: the right treatment for the right patient at the right time.
Our program features:
- Medical oncologists and hematologists who subspecialize in breast cancer
- Access to more than 200 National Cancer Institute-sponsored clinical trials and industry-led studies through our agreement with the internationally recognized Washington University School of Medicine
- One of the nation’s first centers dedicated solely to the treatment of metastatic breast cancer
- Genomic sequencing and precision oncology services for advanced cancers
- A Multidisciplinary Breast Clinic where patients meet with a team of specialists in one comprehensive appointment
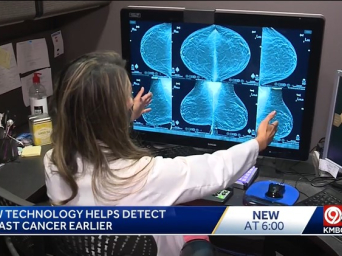
- The region’s largest network of 3-D mammography centers for early detection of the smallest tumors
- Nurse navigators who serve as patient resources and advocates through treatment and beyond
- Supportive Oncology and Rehabilitation Services program to help patients overcome the physical and emotional challenges that often follow diagnosis and treatment
Early Detection
Breast Cancer: Early Detection
You have a better chance of surviving breast cancer if your healthcare provider finds and treats it early, when it’s small and hasn’t spread. The best way to find breast cancer early is to be screened regularly. Screening means being checked before you have any symptoms. Screening isn't possible for many kinds of cancer, but it is with breast cancer. Screening doesn't guarantee that you won't get cancer or die from it, especially if it's found after it has spread. But regular screening may help find the cancer earlier. This is called early detection.
How is screening for breast cancer done?
Screening for breast cancer in women of average risk can include:
-
Breast self-awareness. In the past, a breast self-exam (BSE) was recommended. It was a detailed method of examining your breasts once a month. Most experts now advise breast self-awareness instead. This means having a sense of what's normal for your breasts. If you notice even small changes in how they look or feel, contact your healthcare provider right away.
-
Clinical breast exam (CBE). The American Congress of Obstetricians and Gynecologists (ACOG) advises CBEs every 1 to 3 years for people ages 25 to 39. ACOG advises CBEs every year for people 40 and older. Other experts don't agree that there's enough evidence to say there's a clear benefit of CBEs. Talk with a healthcare provider about your risk factors and decide whether to have a CBE.
-
Mammography. A mammogram is a kind of X-ray used to help find breast tumors before they can be felt or cause other symptoms. During the test, your breast is pressed between two plastic plates that flatten and spread the tissue. Very low levels of radiation are used to take a picture of the inside of your breast. Many facilities have digital mammography. This displays results on a computer instead of on film. The test can be uncomfortable, but it lasts only a few moments. There are more details about mammograms below.
-
Breast MRI. An MRI uses magnets, radio waves, and a computer to make detailed pictures of the inside of the breast. Before the MRI, a contrast dye may be put into your blood through a vein. This helps to better outline the breast tissue and possible tumors. MRI is only used to screen people who are at a high risk for breast cancer based on factors such as family history or genes.
These screening methods can improve your chances of finding cancer early. People at high risk for breast cancer may be advised to start breast cancer screening at a younger age. They may also be advised to have an MRI along with their routine mammograms. For some people with dense breast tissue, ultrasound may be done along with mammograms. Your healthcare provider can tell you more about your risks and what screenings are right for you.
More about mammograms
A mammogram detects tumors and calcium deposits in the breast. Most calcium deposits are not cancer. But a cluster of very tiny specks of calcium (microcalcifications) can be an early sign of breast cancer. If your mammogram shows anything abnormal, you may need more tests.
A mammogram is the best way to find breast cancer early. But it may not always detect cancer. And in some cases, it may find an abnormality that turns out not to be cancer. This is called a false positive.
The benefits and limits of a mammogram vary. They’re based on factors such as age and personal risk. Experts have different advice for who should have mammograms.
-
U.S. Preventive Task Force (USPSTF). This group advises screening every 2 years for people ages 50 to 74. People have the choice to start getting mammograms every 2 years starting at age 40. This should be discussed with a healthcare provider.
-
American Cancer Society (ACS). This group advises yearly screening for all people ages 45 to 54, then a choice of screening every 1 or 2 years for people ages 55 and older. People ages 40 to 45 have the option to start screening.
-
American Congress of Obstetricians and Gynecologists (ACOG). This group advises that starting at age 40, people should have the option of getting mammograms every 1 or 2 years. All people should start at age 50. Mammograms every 1 or 2 years should be done until age 75. At that time, a person should talk with their healthcare provider about whether to continue screening.
All people should talk with their healthcare provider about their personal risk factors and the pros and cons of testing before deciding when to start and how often to get a mammogram.
Grades and Stages
Breast Cancer: Grades and Stages
Once your healthcare provider knows you have breast cancer, the next step is to find out more about your cancer cells. This includes the stage of the cancer, the exact type you have, and other factors. This information is found by doing tests on the cancer cells that were taken out of your body in a procedure called a biopsy.
A lot is known about the biology of breast cancer, like gene changes and other details that make breast cancer cells different from normal cells. In the past, breast cancer was staged based mostly on tumor size and spread (the TNM system). Today, prognostic stage groups are used. These also look at breast cancer cell biomarkers. In fact, these may be even more important than tumor size when deciding things like the best drugs or chemo to use, the value of local (tumor-focused) treatments like radiation, and looking at each woman’s likely outcome (prognosis).
This detailed information allows healthcare providers to use more personalized or focused treatment that’s designed for each woman based on the changes in her cancer cells. But it also makes breast cancer staging very complex.
Here, you'll find more information on the many different factors that are used to find each woman’s breast cancer prognostic stage group. Knowing these details can help you better understand your diagnosis. It can also help you make the treatment decisions that are best for you.
Stages
Stage describes the size of the tumor and how far the cancer has spread in your body. Imaging scans and tests are used to find out the size of the cancer and where it is. These can also show if the cancer has grown into nearby tissues, and if it has spread to other parts of your body.
The most commonly used system to stage breast cancer is the TNM system from the American Joint Committee on Cancer. Here's what the letters stand for in the TNM system:
-
T tells how big the main tumor is and where it is.
-
N tells if the lymph nodes near the original tumor have cancer in them. Lymph nodes are part of the immune system. They help the body fight infections.
-
M tells if the cancer has spread ( metastasized) to distant organs in the body, like the liver, lungs, bones, or brain.
Numbers or letters after T, N, and M provide more details about each of these factors. There are also two other values that can be assigned:
-
X means there's not enough information to assess the extent of the main tumor (TX), or if the lymph nodes have cancer cells in them (NX), or if the cancer has spread to other part of the body (MX).
-
0 means no sign of cancer, such as no sign of spread to the lymph nodes (N0) or other parts of the body (M0).
TNM staging helps determine the type of surgery, if surgery to remove lymph nodes is needed, and if more treatment is needed after surgery.
Grades
The grade refers to how the cancer cells look when compared to normal breast cells. The grade of your cancer helps predict how fast the cancer may grow and spread.
A scale of 1 to 3 is used to grade breast cancer. The lower the number, the more the cancer cells look like normal cells. This means the cancer is less likely to spread and may be easier to treat. Grade 3 cancer cells look very different from normal cells. This grade of cancer is more likely to grow quickly and spread.
Grade is written as G1, G2, and G3. Sometimes GX is used if the grade isn’t known.
HER2 status
HER2 stands for human epidermal growth factor receptor 2. Breast cancer cells that have a lot of this protein are called HER2-positive (HER2+). They tend to grow faster and are more likely to spread to other parts of the body than HER2-negative breast cancers.
There are medicines that target and block HER2 to slow or stop cancer cell growth. If a woman’s breast cancer is HER2+, she should be treated with one of these medicines.
Hormone receptor status
Some breast cancer cells have hormone receptors. When the female hormones estrogen (ER) or progesterone (PR) attach to these receptors, they help the cancer cells grow faster.
Tests can be done to see if a woman’s cancer cells have high amounts of hormone receptors. The results show that the cancer cells are ER-positive or negative (ER+ or ER-) and PR-positive or negative (PR+ or PR-).
This information is used to predict the cancer cell response to medicines that target these hormone receptors. Medicines that block them can slow or stop the growth of the cancer cells. These medicines don’t work on breast cancer cells that are ER-negative and PR-negative.
Prognostic stage groups
All of the above information is put together into what’s called the prognostic stage group. These groupings give an overall description of your cancer.
A prognostic stage group can have a value of 0 to 4, and they're written as Roman numerals 0, I, II, III, and IV. The higher the number, the bigger the cancer is or the more it has spread beyond the breast, or both. Letters are used after the Roman numeral to give more details.
All the details used in prognostic stage grouping help healthcare providers choose the best treatments for each woman and, as a result, get better treatment outcomes. These details also keep women from getting treatments that aren’t needed or won’t work.
Other important factors
Ki-67
Ki-67 is widely used as a marker of cancer cell proliferation. This is how fast the cancer cells are dividing. High Ki-67 levels mean that the cancer cells are dividing fast.
Cancer cell gene tests
Tests that look at patterns of many different gene changes at one time are becoming another important part of managing some breast cancers. But they're not useful for women with HER2+ or triple negative breast cancers.
These tests are often called genomic assays or genomic tests. They look for changes in certain genes in breast cancer cells. The results can be used to help predict likely outcomes after treatment and the need for more treatment after surgery.
The main thing the tests used today show is a woman’s risk of cancer coming back after treatment. For instance, the test may give a recurrence score . This is a measure of the woman’s risk of the cancer coming back in the next 10 years. Other tests may give a risk assessment of how likely it is that the cancer will come back in another part of her body.
Talking with your healthcare provider
Breast cancer staging is very complex. Remember, the key information that’s needed includes:
-
The TNM values
-
Grade
-
HER2 status
-
Hormone-receptor status
Once your cancer is staged, your healthcare provider will talk with you about what the stage means for your treatment. Be sure to ask your healthcare provider to explain the stage of your cancer to you in a way you can understand. Make sure to ask any questions and talk about your concerns so you can make the best decisions about your cancer care.
Risk Factors
Breast Cancer: Risk Factors
What is a risk factor?
A risk factor is anything that may increase your chance of having a disease. Risk factors for a certain type of cancer might include smoking, diet, family history, or many other things. The exact cause of someone’s cancer may not be known. But risk factors can make it more likely for a person to have cancer.
Things you should know about risk factors for cancer:
-
Risk factors can increase a person's risk, but they do not necessarily cause the disease.
-
Some people with one or more risk factors never develop cancer. Other people can develop cancer and have no risk factors.
-
Some risk factors are very well known. But there is ongoing research about risk factors for many types of cancer.
Some risk factors, such as family history, may not be in your control. But others may be things you can change. Knowing the risk factors can help you make choices that might lower your risk. For example, if an unhealthy diet is a risk factor, you may choose to eat healthy foods. If excess weight is a risk factor, your healthcare provider may check your weight or help you lose weight.
Who is at risk for breast cancer?
Risk factors for breast cancer include:
-
Gender. Breast cancer occurs about 100 times more often in women than in men.
-
Race or ethnicity. White people develop breast cancer slightly more often than African-American people. But African-American people tend to die from breast cancer more often. This may be due to differences in access to medical care. This may also be partly due to the fact that African-American people often have a more aggressive type of tumor. (Aggressive tumors grow and spread quickly.) Why this happens is not known. The risk of having breast cancer and dying from it is lower in people who are Hispanic, American Indian, or Asian.
-
Older age. Most people with invasive cancer are older than age 55.
-
History of breast cancer. If you’ve had cancer in one breast, you’re at an increased risk of having it in the other breast or another part of the same breast.
-
Past chest radiation for another cancer. If you’ve had high-dose radiation to your chest, you have an increased chance for breast cancer. The risk is even higher if it happened when you were a child or teen. It’s important to remember that radiation therapy involves high doses of radiation. The small doses used for breast cancer screening do not increase your risk.
-
Family history. Having a parent, sibling, or child with breast cancer increases your risk.
-
Benign breast disease. People with certain noncancer (benign) breast conditions, such as hyperplasia or atypical hyperplasia, have an increased risk for breast cancer. The only way to know if you have benign breast disease and what kind is by having a biopsy.
- Lobular carcinoma in situ (LCIS). LCIS is a noninvasive growth of abnormal cells in the lobules of the breasts (milk-producing glands). LCIS is not considered cancer. But it increases the risk of getting breast cancer. LCIS is typically diagnosed from a biopsy that is done on the breast for another reason.
-
DES ( diethylstilbestrol) exposure. People who took this medicine while pregnant to lower the chance of miscarriage are at higher risk. People whose birth parent took DES during pregnancy with them may also have a slightly higher risk.
-
Early menstrual periods. People whose periods began before age 12 have a slightly higher risk for breast cancer.
-
Late menopause. People are at a slightly higher risk if they began menopause after age 55.
-
Not giving birth to a child, not breastfeeding, or giving birth to your first child after age 30. These people have a slightly higher breast cancer risk.
-
Dense breast tissue. People whose breasts have larger areas of dense tissue on mammograms are at increased risk for breast cancer.
-
Drinking alcohol. Breast cancer risk goes up if you drink just 1 glass of wine, beer, or a mixed drink a day. The more you drink, the higher your risk. Limit yourself to less than 1 drink per day.
-
Long-term use of estrogen and progestin medicines after menopause. This is known as hormone replacement therapy (HRT). The hormones are most often used together. The longer you’ve used HRT, the higher your risk. If you stop taking the medicines, your risk should go back down to normal after 5 years. If you decide to use HRT, use it at the lowest dose and for the shortest time possible.
-
Excess weight, especially after menopause. This risk factor is complex. Research shows conflicting results about the link between weight and breast cancer. Overall, your risk of breast cancer is lower if you stay at a healthy weight with a body mass index (BMI) below 25. If you’re overweight and you get breast cancer, the excess weight also affects your chances of being cured. And it affects your chances of the cancer coming back after treatment.
-
BRCA1 and BRCA2 genes. Certain inherited changes in genes are another risk factor. Hereditary breast cancer accounts for about 1 in 20 to 1 in 10 breast cancer cases. BRCA1 and BRCA2 genes are the most common genes linked to breast cancer. These are tumor suppressor genes that usually have the job of controlling cell growth and cell death. When they're changed, they don't do their job correctly, and cancer tumors may grow. Changes in these genes account for most cases of hereditary breast cancer. They're linked to other kinds of cancer, especially ovarian cancer. In the U.S., BRCA changes are most common in women of Ashkenazi Jewish ancestry.
There are other, less common genes that can impact breast cancer risk.
What are your risk factors?
Talk with your healthcare provider about your risk factors for breast cancer and what you can do about them. There are different tools that can be used to help estimate your risk. These can help you to set up your own best prevention and screening plan.
Providers

Timothy J Pluard, MD

Kelly C Gast, MD

Whitney Lee Hensing, MD

Tammy K Neblock-Beirne, MD
John W Shook, MD

Jacob P Smeltzer, MD